Table of Contents
ToggleClinical objectives for nursing students serve as the roadmap that guides learners from classroom theory to hands-on patient care excellence. These structured goals define what students must accomplish during their clinical rotations, ensuring they develop the competencies needed for safe, effective nursing practice. Well-crafted clinical objectives not only measure student progress but also protect patient safety by establishing clear performance standards.
How Clinical Objectives Bridge Theory and Practice
Clinical objectives for nursing students create essential connections between academic learning and real-world application:
- Translate textbook knowledge into clinical skills – Students apply pathophysiology, pharmacology, and nursing theory concepts directly to patient care situations
- Provide structured learning experiences – Clear objectives ensure students encounter diverse clinical scenarios that build progressive competency
- Create accountability measures – Instructors and students can track skill development and identify areas needing improvement
- Support evidence-based practice – Objectives encourage students to connect current research with bedside decision-making
Five Key Areas This Guide Covers
This comprehensive guide explores the essential components of clinical objectives for nursing students:
- Understanding the framework – Learn what clinical objectives are, how they differ from learning objectives, and why they matter for accreditation and patient safety
- Core competency categories – Explore patient care skills, technical procedures, critical thinking, and communication objectives
- Implementation strategies – Discover how to set SMART goals and track your progress effectively throughout rotations
- Overcoming obstacles – Address common challenges like performance anxiety and knowledge-application gaps
- Maximizing opportunities – Learn best practices for making the most of every clinical experience
Understanding Clinical Objectives in Nursing Education
Clinical objectives form the foundation of nursing education by establishing clear expectations for student performance in healthcare settings. Understanding these objectives helps students approach their clinical rotations with confidence and purpose. This section explores what clinical objectives are, how they differ from other educational standards, and why they’re crucial for both student success and patient safety.
What Clinical Objectives Are and Their Purpose
Clinical objectives for nursing students serve multiple essential functions in healthcare education:
- Define measurable outcomes – Specify exactly what students must demonstrate by the end of each clinical rotation or course
- Guide daily clinical activities – Help students prioritize which skills and experiences to seek during patient care assignments
- Establish evaluation criteria – Provide instructors with concrete standards for assessing student competency and readiness to progress
- Align with professional standards – Reflect the competencies required by state boards of nursing and national healthcare organizations
- Support progressive learning – Build systematically from basic skills to complex clinical reasoning across the curriculum
Worried About Academic Integrity? StudentResearch.net delivers 100% original nursing papers crafted from scratch by expert writers. Every assignment includes a comprehensive plagiarism report, ensuring your work meets the highest academic standards. Trust us for authentic, quality content that protects your reputation.
Difference Between Learning Objectives and Clinical Competencies
| Learning Objectives | Clinical Competencies |
| Focus on knowledge acquisition and understanding | Focus on demonstrated performance and skill application |
| Often classroom-based and theoretical | Always practice-based and hands-on |
| Measured through exams, papers, and discussions | Measured through direct observation and skills assessment |
| Example: “Describe the nursing process” | Example: “Apply the nursing process to patient care” |
| Cognitive emphasis | Psychomotor and affective emphasis |
| Foundation for competency development | End result of integrated learning |
Role of Clinical Objectives in Curriculum Planning
Clinical objectives for nursing students guide the entire structure of nursing programs:
- Sequence clinical experiences logically – Ensure students master foundational skills before advancing to complex patient populations
- Distribute learning across rotations – Allocate medical-surgical, pediatric, psychiatric, and community health experiences appropriately
- Coordinate with coursework – Align clinical placements with concurrent classroom content for reinforced learning
- Meet credit hour requirements – Ensure students receive adequate supervised clinical practice hours for program completion
- Address specialized populations – Guarantee exposure to diverse patient ages, conditions, and healthcare settings
How Clinical Objectives Align with Nursing Program Accreditation Standards
Accreditation bodies require nursing programs to demonstrate student achievement through structured objectives:
- ACEN and CCNE compliance – Programs must document how clinical objectives meet Accreditation Commission for Education in Nursing or Commission on Collegiate Nursing Education standards
- NCLEX preparation – Objectives align with the test plan categories ensuring students develop competencies assessed on licensure exams
- Quality improvement data – Schools track objective achievement rates to identify curriculum strengths and areas needing enhancement
- Employer expectations – Objectives reflect the competencies healthcare facilities expect from newly licensed nurses
- Regional variation accommodation – Allow programs to address specific community health needs while maintaining national standards
The Connection Between Clinical Objectives and Patient Safety
Well-defined clinical objectives for nursing students directly protect patients receiving care:
- Competency verification – Ensure students demonstrate proficiency before performing procedures independently on patients
- Error prevention – Teach students to follow protocols systematically, reducing medication errors and procedural mistakes
- Supervision requirements – Specify which skills require instructor oversight versus independent practice
- Critical thinking development – Train students to recognize early warning signs and respond appropriately to patient deterioration
- Professional accountability – Instill understanding that nursing practice directly impacts patient outcomes and recovery
Core Categories of Clinical Objectives for Nursing Students
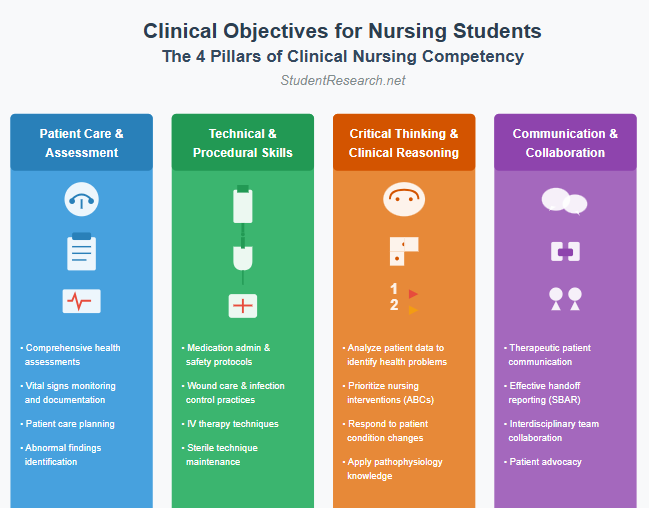
Clinical objectives for nursing students encompass multiple domains that together create competent, safe practitioners. Each category builds essential capabilities that nurses use daily in patient care. Mastering these core areas ensures students graduate prepared for the complex demands of professional nursing practice.
Patient Care and Assessment Skills
Conducting Comprehensive Health Assessments
- Perform head-to-toe physical examinations – Systematically assess all body systems using inspection, palpation, percussion, and auscultation techniques
- Gather complete health histories – Interview patients about current complaints, medical history, medications, allergies, and psychosocial factors
- Identify abnormal findings – Recognize deviations from normal assessment parameters and understand their clinical significance
- Document assessment data accurately – Record findings clearly and concisely in electronic health records using standardized terminology
- Adapt assessment techniques – Modify approaches based on patient age, condition, cultural background, and communication abilities
Performing Vital Signs Monitoring and Documentation
- Measure vital signs accurately – Take blood pressure, pulse, respirations, temperature, oxygen saturation, and pain levels using proper technique
- Recognize critical values – Identify when vital signs fall outside normal ranges and require immediate intervention
- Track trends over time – Monitor changes in vital signs to detect patient improvement or deterioration
- Report abnormalities promptly – Communicate concerning vital signs to charge nurses and physicians according to facility protocols
- Understand clinical context – Interpret vital signs in relation to patient diagnosis, medications, and treatment goals
Developing Patient Care Plans Based on Assessment Findings
- Formulate nursing diagnoses – Analyze assessment data to identify actual and potential health problems using NANDA-I terminology
- Prioritize patient needs – Use frameworks like Maslow’s hierarchy to address life-threatening issues before comfort measures
- Write measurable outcomes – Create specific, time-bound goals that define expected patient improvements
- Select evidence-based interventions – Choose nursing actions supported by current research and best practice guidelines
- Evaluate plan effectiveness – Reassess patients regularly to determine if interventions are achieving desired outcomes
Technical and Procedural Competencies
Medication Administration and Safety Protocols
- Apply the six rights consistently – Verify right patient, medication, dose, route, time, and documentation before every administration
- Calculate dosages accurately – Perform mathematical conversions and dosage calculations, especially for high-risk medications
- Understand pharmacological actions – Explain why medications are prescribed, their therapeutic effects, and potential adverse reactions
- Monitor for drug interactions – Recognize when multiple medications may interact dangerously and alert prescribers
- Educate patients about medications – Teach patients about their drugs’ purposes, side effects, and special administration requirements
Wound Care and Infection Control Practices
- Assess wounds systematically – Evaluate size, depth, drainage, tissue type, and signs of infection using standardized assessment tools
- Select appropriate dressings – Choose wound care products based on wound characteristics and healing phase
- Maintain sterile technique – Perform procedures using aseptic principles to prevent healthcare-associated infections
- Implement isolation precautions – Follow standard, contact, droplet, and airborne precautions based on patient diagnoses
- Practice hand hygiene rigorously – Perform handwashing and alcohol-based hand rub at all required moments during patient care
IV Therapy and Catheterization Techniques
- Insert peripheral IV catheters – Successfully establish venous access using proper vein selection and insertion techniques
- Monitor IV sites and infusions – Assess for complications like infiltration, phlebitis, and infection during IV therapy
- Calculate IV drip rates – Determine correct flow rates for gravity and pump-controlled infusions
- Insert urinary catheters safely – Perform catheterization using sterile technique while maintaining patient dignity
- Provide catheter care – Prevent catheter-associated urinary tract infections through evidence-based maintenance practices
Critical Thinking and Clinical Reasoning
Analyzing Patient Data to Identify Health Problems
- Synthesize multiple data sources – Integrate assessment findings, laboratory results, imaging reports, and patient history into comprehensive pictures
- Recognize patterns and clusters – Identify when seemingly unrelated symptoms indicate specific syndromes or complications
- Question inconsistencies – Notice when data doesn’t align with expected findings and investigate discrepancies
- Consider differential diagnoses – Think broadly about possible causes of patient symptoms before narrowing to most likely explanations
- Apply pathophysiology knowledge – Connect disease processes to clinical manifestations observed in patients
Prioritizing Nursing Interventions Appropriately
- Use the ABCs framework – Address airway, breathing, and circulation issues before other concerns
- Distinguish urgent from important – Determine which tasks require immediate action versus those that can wait
- Consider multiple patients – Allocate time and attention appropriately when caring for several patients simultaneously
- Anticipate complications – Implement preventive interventions for patients at high risk for specific problems
- Reassess priorities continuously – Adjust plans as patient conditions and unit situations change throughout shifts
Responding to Changes in Patient Conditions
- Recognize early warning signs – Detect subtle changes indicating patient deterioration before emergencies develop
- Initiate rapid response protocols – Activate appropriate emergency teams when patients show concerning changes
- Perform emergency interventions – Provide CPR, bag-valve-mask ventilation, and other life-saving measures competently
- Communicate clearly during crises – Use SBAR (Situation-Background-Assessment-Recommendation) format for urgent reporting
- Document response actions – Record timeline of events, interventions performed, and patient responses during emergencies
Communication and Interprofessional Collaboration
Therapeutic Communication with Patients and Families
- Establish trusting relationships – Use active listening, empathy, and genuine presence to build rapport with patients
- Ask open-ended questions – Encourage patients to share concerns fully rather than limiting them to yes/no responses
- Provide patient education effectively – Teach using appropriate language level, visual aids, and teach-back methods to confirm understanding
- Address emotional needs – Recognize and respond to patient anxiety, fear, grief, and other emotional responses to illness
- Navigate difficult conversations – Discuss sensitive topics like end-of-life preferences, non-adherence, and lifestyle changes with compassion
Effective Handoff Reporting and Documentation
- Give organized shift reports – Present patient information systematically including diagnosis, current status, pending tasks, and concerns
- Document comprehensively – Chart nursing assessments, interventions, patient responses, and teaching in electronic health records
- Use standardized handoff tools – Apply SBAR or I-PASS frameworks to ensure complete information transfer between providers
- Highlight critical information – Emphasize changes in condition, abnormal lab results, and time-sensitive interventions during handoffs
- Maintain confidentiality – Share patient information only with authorized healthcare team members in appropriate settings
Collaborating with Interdisciplinary Healthcare Teams
- Participate in team rounds – Contribute nursing perspectives during interdisciplinary discussions about patient care plans
- Coordinate with multiple departments – Work effectively with physicians, therapists, social workers, pharmacists, and other professionals
- Advocate for patient needs – Speak up when care plans don’t address patient concerns or when orders seem inappropriate
- Respect professional boundaries – Understand the scope of practice for various team members while valuing each role
- Resolve conflicts constructively – Address disagreements professionally focusing on patient welfare rather than personal preferences
Setting and Achieving Effective Clinical Objectives
Establishing clear clinical objectives for nursing students provides direction and motivation throughout demanding clinical rotations. Success requires intentional goal-setting combined with systematic progress tracking. This section offers practical strategies for creating meaningful objectives and achieving them through focused effort and reflection.
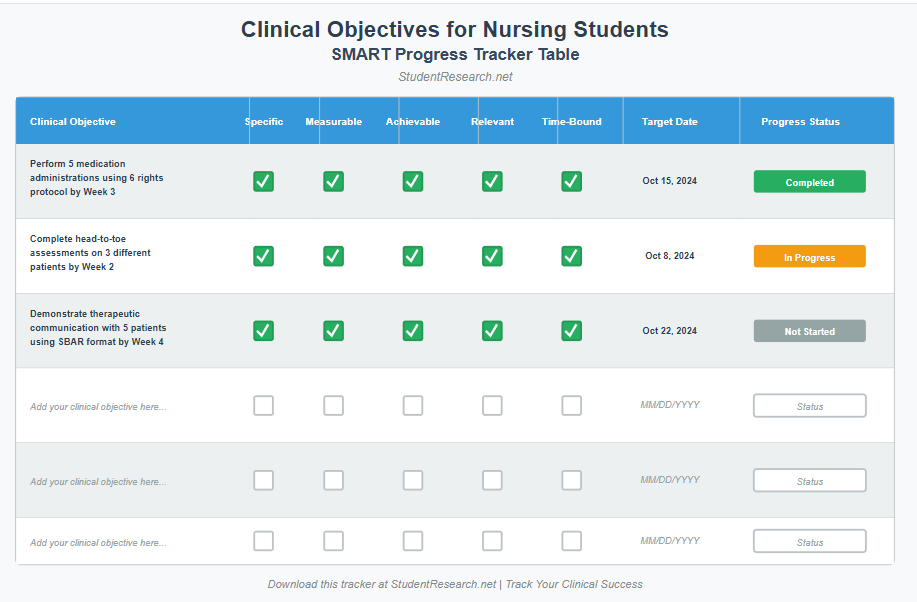
SMART Criteria for Clinical Objective Development
- Specific objectives target concrete skills – “Administer oral medications safely to five patients” rather than “improve medication skills”
- Measurable outcomes allow progress tracking – Include numbers, frequencies, or percentages that indicate achievement levels
- Achievable goals match current ability – Set objectives slightly beyond comfort zones but within reach with reasonable effort
- Relevant objectives align with rotation focus – Prioritize objectives matching the clinical setting, such as pediatric assessment in pediatric rotations
- Time-bound targets create urgency – Specify completion deadlines like “by week four of rotation” to maintain momentum
Creating Personalized Clinical Learning Goals
- Assess current competency levels honestly – Identify which skills you’ve mastered versus those needing improvement through self-reflection
- Consider career interests – Focus additional attention on specialties you might pursue, such as critical care or obstetrics
- Address previous evaluation feedback – Target areas instructors identified as needing development in past clinical experiences
- Balance diverse skill categories – Set goals across technical skills, communication, critical thinking, and professional behaviors
- Discuss goals with clinical instructors – Share objectives with supervisors who can create opportunities for skill practice
Need Help at 2 AM Before Clinical? StudentResearch.net offers round-the-clock support for nursing students worldwide. Whether you need urgent consultations, quick revisions, or last-minute assistance, our expert team is available 24/7 across all time zones. Get the help you need, whenever you need it.
Strategies for Tracking Progress Throughout Clinical Rotations
- Maintain a clinical skills checklist – Record each time you perform procedures to document growing experience and confidence
- Keep a clinical journal – Write weekly reflections describing what you learned, challenges encountered, and progress made
- Request mid-rotation feedback – Ask instructors for formal evaluations at rotation midpoints rather than waiting until the end
- Review objectives weekly – Assess which goals you’ve achieved and which require additional focus in remaining clinical days
- Collect specific examples – Note particular patient situations where you successfully demonstrated targeted competencies
Working with Clinical Instructors and Preceptors
- Communicate objectives proactively – Share your personal goals during initial meetings so instructors can facilitate relevant experiences
- Ask for teaching moments – Request that instructors demonstrate techniques before you attempt them independently
- Seek constructive criticism – Invite feedback on your performance, viewing suggestions as growth opportunities rather than criticisms
- Prepare questions in advance – Come to clinical with specific questions about concepts or procedures you want to understand better
- Express gratitude and receptiveness – Show appreciation for instructor guidance and demonstrate willingness to implement their suggestions
Using Reflection Journals and Self-Assessment Tools
- Describe significant patient encounters – Write detailed accounts of memorable cases including your nursing actions and patient outcomes
- Analyze clinical reasoning processes – Explain why you made particular decisions and what you would do differently next time
- Identify emotional responses – Acknowledge feelings about challenging situations like patient deaths or difficult family interactions
- Connect theory to practice – Link classroom concepts to clinical experiences showing how knowledge applies in real settings
- Track confidence growth – Note which procedures initially intimidated you but now feel manageable through repeated practice
Common Challenges and Best Practices
Even the most dedicated nursing students encounter obstacles during their clinical education journey. Recognizing common challenges helps students prepare strategies to overcome them effectively. This final section addresses typical difficulties students face and shares evidence-based practices for maximizing every clinical learning opportunity.
Overcoming Clinical Learning Obstacles
Managing Performance Anxiety in Clinical Settings
- Acknowledge nervousness as normal – Recognize that feeling anxious about clinical performance is universal among nursing students, not a sign of inadequacy
- Practice skills in simulation labs – Build confidence through repetition in low-stakes environments before performing procedures on actual patients
- Use positive self-talk – Replace thoughts like “I’ll mess this up” with “I’ve practiced this and my instructor is here to help”
- Focus on the present moment – Concentrate on the current task rather than worrying about future evaluations or past mistakes
- Develop pre-clinical routines – Create calming rituals like reviewing notes or deep breathing exercises before clinical days begin
Addressing Gaps Between Classroom Knowledge and Clinical Application
- Review theory before clinical days – Read about diagnoses and procedures you’ll likely encounter during upcoming shifts
- Ask “why” questions constantly – Connect bedside tasks to underlying pathophysiology by questioning the rationale for every intervention
- Request real-time explanations – When confused about procedures, ask instructors to explain the connection to classroom concepts immediately
- Study actual patient cases – After clinical days, research your patients’ conditions more deeply to solidify understanding
- Form study groups with peers – Discuss clinical experiences together to learn from each other’s patient encounters and insights
Building Confidence Through Progressive Responsibility
- Start with observation – Watch experienced nurses perform complex skills before attempting them yourself
- Practice with supervision first – Perform procedures under direct instructor oversight until you demonstrate consistent competency
- Gradually increase independence – Take on more patients and complex care situations as your skills develop
- Volunteer for challenging assignments – Seek patients with unfamiliar conditions or difficult procedures to expand your capabilities
- Celebrate small victories – Acknowledge each successful skill performance and positive patient interaction as evidence of growing competence
Maximizing Clinical Learning Opportunities
Being Proactive in Seeking Diverse Patient Experiences
- Request varied patient assignments – Ask instructors for patients with different diagnoses, ages, and complexity levels across rotations
- Explore different units – Spend observation time in specialty areas like ICU, emergency department, or operating rooms when possible
- Attend procedures with patients – Accompany your patients to radiology, surgery, or other departments to see the full care continuum
- Learn from every patient – Even “routine” patients offer opportunities to refine communication skills and time management abilities
- Shadow different nursing roles – Observe charge nurses, nurse educators, and case managers to understand career possibilities
Preparing for Clinical Days Through Case Study Review
- Research common conditions – Study the typical diagnoses seen in your assigned unit before beginning each new rotation
- Review medication protocols – Familiarize yourself with frequently administered drugs including dosages, side effects, and nursing considerations
- Practice assessment techniques – Rehearse physical examination skills at home or in lab to perform them smoothly with patients
- Prepare questions in advance – Write down concepts you want to clarify so you remember to ask instructors during clinical time
- Organize clinical tools – Keep reference cards, assessment forms, and drug guides readily accessible in your uniform pockets
Asking Questions and Seeking Feedback Regularly
- Question everything respectfully – Inquire about rationales, alternatives, and evidence behind nursing interventions you observe
- Request immediate performance feedback – After completing procedures, ask instructors how you did and what to improve next time
- Seek clarification without hesitation – Never proceed with actions you don’t fully understand; patient safety depends on your certainty
- Learn from mistakes openly – When errors occur, discuss them honestly with instructors to prevent repetition
- Ask for growth suggestions – Regularly request specific recommendations for strengthening your weakest skill areas
Connecting Clinical Experiences to Evidence-Based Practice
- Question routine practices – Consider whether traditional nursing interventions reflect current research or simply “how it’s always been done”
- Look up recent studies – Search nursing journals for evidence supporting or challenging the interventions you observe in clinical settings
- Discuss research during post-conferences – Share interesting evidence-based findings with clinical groups to promote critical thinking
- Apply research to care plans – Cite current evidence when selecting nursing interventions for your assigned patients
- Participate in unit quality improvement – Contribute to evidence-based practice initiatives happening on your clinical units
Conclusion
Clinical objectives for nursing students provide the essential framework that transforms eager learners into competent, confident nursing professionals. These carefully structured goals ensure students develop patient care skills, technical competencies, critical thinking abilities, and strategies for clinical success needed to deliver safe, effective care. By understanding what clinical objectives are, mastering core competency categories, implementing SMART goal-setting strategies, overcoming common obstacles, and maximizing every learning opportunity, nursing students position themselves for excellence in both their education and future careers.
Meeting clinical objectives for nursing students does more than fulfill graduation requirements—it prepares you for the NCLEX licensure examination and the realities of professional nursing practice. The assessment skills, technical procedures, clinical reasoning abilities, and communication competencies you develop through structured clinical objectives become the foundation of your nursing practice throughout your entire career. Every objective achieved represents not just a checked box but a life-saving skill you’ll use to positively impact patient outcomes.
The journey from nursing student to competent professional requires dedication, resilience, and continuous learning. Embrace each clinical rotation as an opportunity to grow, view challenges as learning experiences rather than failures, and remember that even the most accomplished nurses once stood exactly where you are now. Your commitment to mastering clinical objectives for nursing students demonstrates the professional accountability and patient-centered focus that defines excellent nursing care. Continue approaching your clinical education with curiosity, humility, and determination—these qualities will serve you well throughout your nursing career.
Drowning in Clinical Hours AND Assignment Deadlines? StudentResearch.net guarantees on-time delivery for every nursing paper, including rush orders. We understand your demanding schedule and respect your submission deadlines. Focus on mastering clinical objectives while we handle your academic writing with reliable, punctual service.