Table of Contents
ToggleWhy Every Nursing Student Needs Trauma Informed Care Training Now
Picture this: You’re on your first clinical rotation, and a patient suddenly becomes agitated during a routine procedure. What you didn’t know was that this patient was a survivor of medical trauma, and the approach used inadvertently re-traumatized them. This scenario underscores why trauma informed care podcast for nursing students has become essential listening for those entering the profession.
Approximately 70% of adults have experienced at least one traumatic event in their lifetime. As future healthcare providers, nursing students must understand that trauma isn’t just a psychological concept—it’s a lens through which we must view every patient interaction. The trauma informed care podcast for nursing students movement represents a paradigm shift in how we prepare the next generation of nurses to deliver compassionate, effective care.
This comprehensive guide will walk you through nine critical mastery skills that every nursing student should develop, supported by practical templates, real-world examples, and evidence-based strategies. Whether you’re just beginning your nursing journey or preparing for clinical practice, understanding trauma informed care through accessible podcast education can transform not only your patient outcomes but your entire approach to healthcare delivery.
#1 – Understanding the Foundations: What Makes Trauma Informed Care Essential
Trauma informed care (TIC) represents a fundamental shift from asking “What’s wrong with you?” to “What happened to you?” This reframing acknowledges that behaviors stem from adaptive responses to traumatic experiences rather than character flaws. For nursing students, grasping this foundation through dedicated trauma informed care podcast for nursing students resources creates a framework for understanding complex patient presentations throughout their careers.
SAMHSA identifies six key principles: safety, trustworthiness and transparency, peer support, collaboration and mutuality, empowerment and choice, and cultural considerations. Student research demonstrates that when these principles are applied in clinical settings, patient satisfaction scores increase, medical adherence improves, and healthcare providers report greater job satisfaction.
The Six Core Principles Explained
Safety Principle:
- Physical safety in the environment (lighting, exits, private spaces)
- Emotional safety in interactions (predictability, consistency, boundaries)
- Psychological safety in communication (non-judgmental language, patient autonomy)
Trustworthiness and Transparency:
- Clear communication about procedures and expectations
- Following through on commitments made to patients
- Honest acknowledgment when mistakes occur
Peer Support and Collaboration:
- Recognizing the value of lived experience
- Facilitating connections between patients with similar backgrounds
- Mutual decision-making processes
The Evidence Base Supporting Trauma Informed Approaches
| Study Focus | Key Finding | Patient Impact | Healthcare System Impact |
|---|---|---|---|
| Emergency Department TIC | 42% reduction in escalation incidents | Decreased re-traumatization | Lower security calls |
| Primary Care TIC Training | 67% increase in trauma screening | Earlier intervention | Improved chronic disease outcomes |
| Pediatric Hospital TIC | 53% reduction in restraint use | Less invasive interventions | Cost savings |
| Mental Health Integration | 71% improvement in treatment engagement | Better long-term outcomes | Decreased emergency utilization |
Need help citing trauma research for your nursing papers? StudentResearch.net specializes in evidence-based academic writing for nursing students. Our healthcare-focused writers deliver properly referenced, plagiarism-free assignments that meet your program’s rigorous standards. Quality guaranteed, deadlines respected.
#2 – Recognizing Trauma Responses in Clinical Settings
Every nursing student will encounter patients exhibiting trauma responses, often without realizing the underlying cause. Learning to recognize these responses through trauma informed care podcast for nursing students education equips future nurses with observational skills necessary for appropriate intervention.
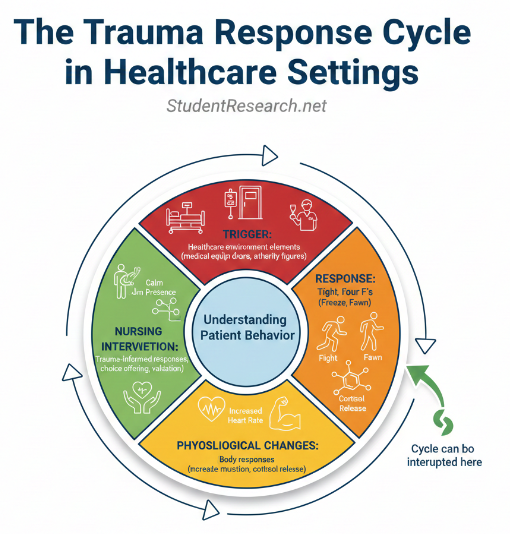
The human nervous system responds to perceived threat through four pathways: fight, flight, freeze, and fawn. Student research indicates that healthcare providers who cannot accurately identify these responses often misinterpret patient behavior as difficult or non-compliant, leading to interventions that escalate rather than de-escalate situations.
The Four F’s of Trauma Response
Fight Response Indicators:
- Verbal aggression or raised voice
- Physical tension or threatening posture
- Argumentative behavior
- Refusal to cooperate with procedures
Flight Response Indicators:
- Attempts to leave against medical advice
- Frequent discharge requests
- Avoidance of eye contact
- Restlessness and inability to remain still
Freeze Response Indicators:
- Dissociation or “spacing out”
- Flat affect or emotional numbness
- Non-responsiveness to questions
- Physical stillness or rigidity
Fawn Response Indicators:
- Excessive agreement or compliance
- Apologizing excessively
- Difficulty expressing needs
- People-pleasing behaviors
Common Triggers in Healthcare Environments
Physical Environment Triggers:
- Closed doors or lack of visible exits
- Vulnerable positions (lying down, undressed)
- Bright lights or loud noises
- Institutional smells
Procedural Triggers:
- Loss of control over one’s body
- Painful or invasive procedures
- Touch without warning
- Restraints or restricted movement
#3 – Essential Communication Skills from Expert Podcast Interviews
Communication forms the cornerstone of trauma informed care, and trauma informed care podcast for nursing students platforms frequently feature communication experts sharing strategies for clinical settings. The way nursing students introduce themselves, explain procedures, and respond to distress directly impacts whether patients feel safe or threatened.
Student research examining patient satisfaction reveals that patients consistently rate “feeling heard” and “being treated with respect” as more important than technical skill. This underscores why mastering trauma informed communication is a clinical competency, not a soft skill.
The Power of Transparent Communication
Before Procedures:
- “I’m going to explain exactly what will happen before we begin”
- “You can ask me to stop at any time”
- “Let me know if anything feels uncomfortable”
During Patient Care:
- “I’m going to touch your arm now to check your blood pressure”
- “I notice you seem uncomfortable—can you tell me more?”
- “What would help you feel safer right now?”
When Patients Are Distressed:
- “You’re safe here. I’m [name] and I’m a nursing student”
- “I can see this is difficult. What do you need from me?”
- “There’s no rush. We can take this at whatever pace works for you”
Active Listening Techniques for Trauma Survivors
Reflective Listening:
- “What I’m hearing is that you’re worried about…”
- “It sounds like this experience reminds you of…”
- “Let me make sure I understand correctly…”
Validation Statements:
- “That must have been incredibly difficult”
- “Your feelings are completely understandable”
- “Thank you for trusting me with this information”
Empowering Questions:
- “What has helped you feel safe in the past?”
- “How would you like me to support you through this?”
- “What information would be most helpful right now?”
Struggling with nursing assignments while mastering trauma informed care? StudentResearch.net connects you with expert academic writers who understand healthcare education. Get professionally crafted papers, case studies, and research projects delivered on time—so you can focus on clinical excellence.
#4 – Creating Safe Spaces: Environmental Modifications That Matter
The physical environment can either support or undermine trauma informed care efforts. Trauma informed care podcast for nursing students often includes interviews with healthcare designers explaining how small modifications profoundly impact patient comfort and safety.
Student research examining patient feedback reveals consistent themes: patients feel most safe with visual access to exits, control over lighting and temperature, privacy for sensitive conversations, and predictable routines. While nursing students may not control facility design, understanding these principles allows modifications within their scope of practice.
Physical Space Considerations
Patient Rooms:
- Adjustable lighting controls accessible to patients
- Temperature controls within patient reach
- Positioning beds to allow patients to see the door
- Whiteboards with daily schedule and care team names
Examination Rooms:
- Gowns that provide adequate coverage
- Mirror availability so patients can observe procedures
- Step stools to reduce vulnerability
- Modesty screens or curtains
Privacy and Dignity Protocols
| Privacy Element | Trauma Informed Approach | Patient Impact |
|---|---|---|
| Gowning procedures | Explain why needed, offer alternatives | Reduced vulnerability |
| Physical examinations | Expose only necessary areas, re-cover promptly | Maintained dignity |
| Door management | Keep closed, knock before entering | Increased safety |
| Conversation volume | Quiet discussions of sensitive topics | Protected confidentiality |
#5 – Mastering De-escalation Techniques Through Podcast Case Studies
De-escalation represents one of the most critical skills nursing students can develop, and trauma informed care podcast for nursing students provides access to real-world scenarios illustrating both successful and unsuccessful attempts. Unlike restraint or sedation, de-escalation respects patient autonomy while ensuring safety.
Student research on de-escalation effectiveness shows that interventions targeting the autonomic nervous system—through calm presence, predictable responses, and restoration of choice—are significantly more effective than those attempting to logically persuade someone in a heightened emotional state.
The De-escalation Continuum
Stage 1: Early Recognition
- Recognize early warning signs (raised voice, pacing, withdrawal)
- Approach calmly and introduce yourself
- Ask open-ended questions: “What’s going on?”
- Validate feelings: “I can see you’re upset”
- Offer choices: “Would you like to talk here or somewhere more private?”
Stage 2: Active De-escalation
- Maintain calm, non-threatening body language
- Lower your voice and slow your speech
- Create space—don’t crowd or corner
- Focus on immediate concern, not the behavior
- Reflect and validate: “This situation is frustrating”
Stage 3: Crisis Management
- Ensure safety first—yours, patient’s, and others’
- Call for additional support if needed
- Continue calm, reassuring presence
- Offer concrete support: “I’m here with you”
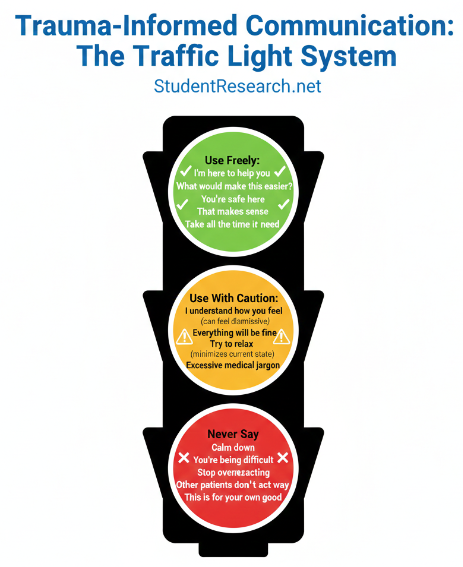
De-escalation Language Templates
DO Say:
- “I’m here to help you”
- “Let’s work on this together”
- “What would make this easier?”
- “You’re safe here”
- “That makes sense”
DON’T Say:
- “Calm down” or “Relax”
- “You’re being difficult”
- “You need to cooperate”
- “Stop overreacting”
#6 – Cultural Competency and Trauma: Insights from Diverse Nursing Voices
Trauma informed care cannot be separated from cultural competency, as trauma’s impact is shaped by cultural context and historical oppression. Trauma informed care podcast for nursing students featuring diverse nursing voices provide essential perspective on how cultural identity intersects with trauma.
Student research on health disparities reveals that marginalized communities experience disproportionate rates of both traumatic experiences and re-traumatization within healthcare systems. Indigenous communities face intergenerational trauma from colonization; Black Americans navigate ongoing systemic racism; LGBTQ+ individuals frequently encounter discrimination in healthcare.
Historical Trauma and Healthcare Mistrust
| Community | Historical Trauma | Trauma Informed Response |
|---|---|---|
| Black/African American | Slavery, Tuskegee experiment | Acknowledge history, emphasize consent |
| Indigenous/Native American | Forced relocation, boarding schools | Respect traditional healing, cultural liaisons |
| Latinx/Hispanic | Immigration trauma, family separation | Confidentiality assurance, language access |
| LGBTQ+ | Conversion therapy, pathologization | Inclusive language, visible affirmation |
Addressing Implicit Bias in Trauma Care
Self-Awareness Practices:
- Regular implicit bias testing and reflection
- Examining assumptions about patient credibility
- Noticing differential treatment patterns
- Seeking feedback from diverse colleagues
- Engaging in ongoing cultural humility education
#7 – Self-Care for Student Nurses: Preventing Vicarious Trauma
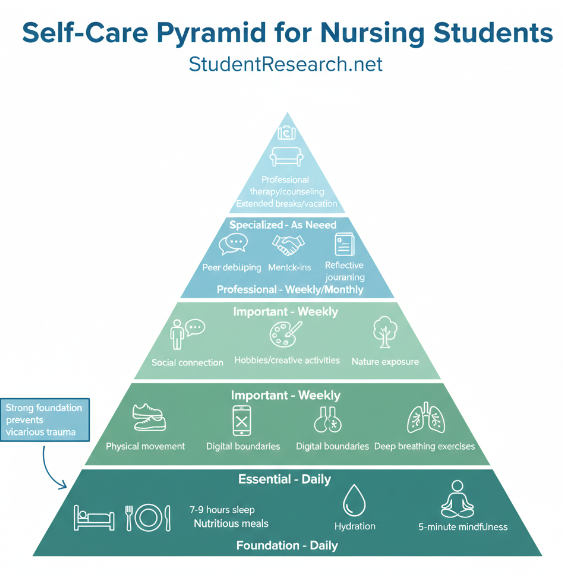
Nursing students learning trauma informed care through trauma informed care podcast for nursing students must simultaneously protect their own wellbeing. Vicarious trauma occurs when exposure to others’ traumatic experiences affects the healthcare provider’s own mental health.
Student research reveals that up to 40% of nursing students report burnout symptoms before graduation. Those exposed to high levels of patient trauma without adequate support are at increased risk for anxiety, depression, and leaving the profession, making self-care a professional necessity.
Recognizing Vicarious Trauma Symptoms
Emotional Symptoms:
- Feeling emotionally numb or overwhelmed
- Difficulty separating work stress from personal life
- Reduced empathy or compassion for patients
Physical Symptoms:
- Sleep disturbances or nightmares
- Changes in appetite
- Fatigue despite adequate rest
Behavioral Symptoms:
- Social withdrawal or isolation
- Overworking or inability to take breaks
- Avoiding certain patients or situations
Evidence-Based Self-Care Strategies
Daily Practices:
- Mindfulness meditation (even 5 minutes)
- Physical movement or exercise
- Adequate sleep hygiene (7-9 hours)
- Digital boundaries (especially before bed)
Weekly Practices:
- Debriefing with trusted colleagues or mentors
- Engaging in enjoyable non-nursing activities
- Social connection with supportive friends/family
- Professional therapy or counseling
#8 – Trauma Informed Documentation and Handoff Communication
Documentation represents a crucial yet often overlooked aspect of trauma informed care. Trauma informed care podcast for nursing students addressing documentation help students understand how written and verbal communication can either perpetuate stigma or support recovery-oriented care.
The language nursing students use in charting and handoff reports shapes how other healthcare providers perceive and interact with patients. Student research analyzing nursing documentation reveals that stigmatizing language—describing patients as “difficult” or “non-compliant”—frequently appears in charts of trauma survivors.
Language Matters: Documentation Do’s and Don’ts
Instead of: “Difficult patient” Use: “Patient expressing distress”
Instead of: “Non-compliant with medications” Use: “Patient reports difficulty maintaining medication schedule”
Instead of: “Manipulative behavior” Use: “Patient attempting to meet needs through [describe behavior]”
Instead of: “Drug-seeking” Use: “Patient reports uncontrolled pain”
H3: Trauma Informed Handoff Reports (SBAR Adaptation)
S – Situation: “This is [patient name], who has a history of medical trauma and prefers [specific approaches]”
B – Background: “Patient reports past negative healthcare experiences with [specific triggers]. They respond well to [communication style]”
A – Assessment: “Patient is currently experiencing anxiety. They have requested [specific accommodation]”
R – Recommendation: “Suggest explaining all steps before beginning and offering breaks”
#9 – Implementing Trauma Informed Care in Clinical Rotations
The transition from learning about trauma informed care through trauma informed care podcast for nursing students to implementing these principles in real clinical settings represents a critical juncture. Student research examining this transition reveals barriers including time pressures, unsupportive preceptors, and institutional cultures that don’t prioritize trauma informed approaches.
However, nursing students who successfully integrate trauma informed care report greater satisfaction, improved patient relationships, and enhanced critical thinking skills. The key lies in starting small and focusing on what you can control.
Starting Small: Micro-Interventions for Every Patient
Pre-Interaction Preparation:
- Review chart for trauma indicators
- Take three deep breaths to center yourself
- Set intention for trauma informed presence
- Remind yourself: “What happened to you?”
During Every Patient Interaction:
- Knock before entering, introduce yourself clearly
- Explain what you’ll be doing before you do it
- Ask permission before touching
- Offer choices whenever possible
- Notice patient’s comfort level and adjust
Overcoming Common Implementation Barriers
| Barrier | Trauma Informed Solution |
|---|---|
| Time constraints | Front-load explanations to reduce patient anxiety and subsequent questions |
| Skeptical colleagues | Focus on outcomes, share evidence, lead by example |
| Difficult patients | Recognize trauma responses, adjust approach |
| Lack of training | Utilize podcast resources, online modules, mentors |
Recommended Trauma Informed Care Podcasts and Resources
Specific high-quality podcast recommendations can jumpstart your learning journey. The trauma informed care podcast for nursing students landscape has expanded significantly, offering numerous options for engaging with this content.
Top Podcast Recommendations
General Trauma Informed Care:
- “Trauma Informed Everything”
- “The Trauma Therapist Podcast”
- “Trauma Healing Accelerated”
Nursing-Specific Podcasts:
- “The Nursing Beat”
- “Happy Hour with Nurses”
- “The Nurse Keith Show”
Supplementary Learning Resources
Free Online Courses:
- SAMHSA’s Trauma-Informed Care in Behavioral Health Services
- ACEs Aware Initiative Training Modules
- National Child Traumatic Stress Network Learning Center
Essential Books:
- “The Body Keeps the Score” by Bessel van der Kolk
- “What Happened to You?” by Bruce Perry and Oprah Winfrey
- “Compassionomics” by Trzeciak and Mazzarelli
Overwhelmed balancing clinical rotations and coursework? StudentResearch.net offers custom writing services tailored to nursing students’ unique needs. From care plans to capstone projects, our specialists ensure your academic work reflects trauma informed principles and professional standards. Confidential and reliable.
Conclusion – Your Journey Toward Trauma Informed Nursing Excellence
As you’ve discovered throughout this guide, trauma informed care podcast for nursing students represents far more than an educational trend—it’s a gateway to transforming your nursing practice from task-oriented care to truly therapeutic, patient-centered healing. The nine mastery skills we’ve explored provide a roadmap for developing competencies that will define you as a nurse who honors the whole person.
The evidence demonstrates that trauma informed care improves patient outcomes, enhances healthcare team satisfaction, and reduces costs. More importantly, it aligns nursing practice with core values: compassion, advocacy, healing, and human dignity. By engaging with trauma informed care podcast for nursing students resources and consistently applying these principles, you’re joining a movement reshaping healthcare delivery.
Remember that becoming trauma informed is not a destination but a continuous journey. The templates, examples, and strategies provided offer starting points. Start today by subscribing to your first trauma informed care podcast for nursing students, implementing one micro-intervention in your next patient interaction, and committing to asking “What happened to you?” rather than “What’s wrong with you?”
As noted in the preceeding sections trauma informed care podcast for nursing students: Discover 9 mastery skills, real examples & templates to transform your practice with expert guidance.