Table of Contents
ToggleWhy Reflective Practice Matters for Nursing Students
You’ve just completed your first independent medication administration, and your mind races with questions about your performance. This is where nursing student reflection examples become invaluable for transforming clinical experiences into professional growth. Quality nursing student reflection examples bridge the gap between classroom theory and bedside reality, developing the critical thinking skills essential for patient care. Nursing student reflection examples show how experienced learners process challenging situations, analyze their responses, and create improvement plans.
Reflective practice is more than an academic requirement—it’s a fundamental skill that separates competent nurses from exceptional ones. Student research shows that nurses who engage in regular reflection demonstrate stronger clinical judgment and better patient outcomes throughout their careers.
This guide provides practical nursing student reflection examples across six critical areas of nursing education, including patient care interactions, technical skills, communication challenges, ethical dilemmas, and self-care strategies. Each example illustrates essential reflection components: detailed descriptions, honest emotional responses, theory-to-practice connections, and specific action plans. Student research demonstrates that consistent reflective practice enhances clinical reasoning and builds the professional resilience necessary for healthcare success.
How to Write a Nursing Reflection: Key Components and Models
Writing an effective nursing reflection requires more than simply describing what happened during your clinical shift. A strong reflection demonstrates deep analysis, connects theoretical knowledge to practical application, and identifies specific areas for growth. Understanding the key components and established reflective models will help you structure your thoughts coherently and extract maximum learning from every clinical experience. Mastering these foundational elements transforms ordinary journal entries into powerful professional development tools.
Essential Elements of Effective Nursing Student Reflections
Every quality nursing reflection contains specific elements that work together to create a comprehensive learning experience. These components guide you through systematic analysis of your clinical encounters.
Core Reflection Components
- Description of the clinical experience: Provide context including the setting, patient demographics, and your specific role in the situation without breaching confidentiality
- Emotional responses and feelings: Honestly acknowledge how the experience made you feel, whether anxious, confident, overwhelmed, or satisfied with your performance
- Critical evaluation and analysis: Examine what went well, what could have been improved, and why certain outcomes occurred based on your actions
- Theory-to-practice connections: Link your experience to nursing theories, evidence-based research, pharmacology principles, or pathophysiology concepts learned in class
- Self-assessment and growth areas: Identify specific competencies you demonstrated and skills requiring further development with concrete examples
- Action plan for future practice: Outline measurable steps you’ll take to improve, including additional reading, skills practice, or mentorship opportunities
Reflective Models for Nursing Students
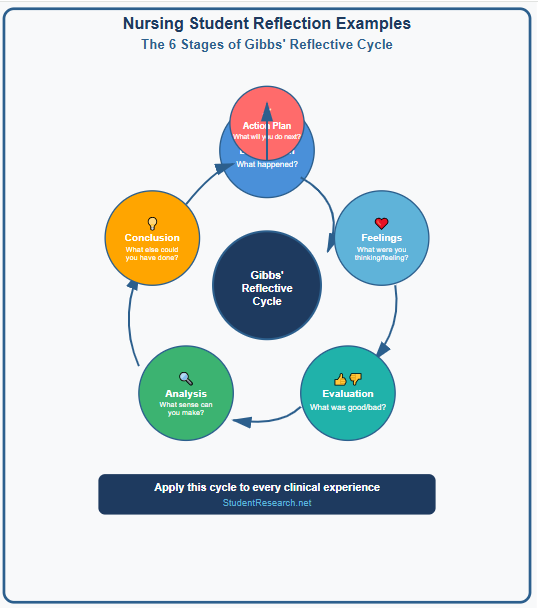
Structured frameworks help organize your thoughts and ensure comprehensive reflection. Each model offers a slightly different approach to processing clinical experiences.
- Gibbs’ Reflective Cycle: Six-stage model including description, feelings, evaluation, analysis, conclusion, and action plan—ideal for complex situations
- Kolb’s Experiential Learning Cycle: Four-stage process emphasizing concrete experience, reflective observation, abstract conceptualization, and active experimentation
- Johns’ Model of Structured Reflection: Cue-question approach focusing on aesthetics, personal knowing, ethics, and empirical knowledge
- Driscoll’s “What? So What? Now What?” model: Simplified three-stage framework perfect for beginners or brief reflections
Choosing the Right Reflection Framework for Your Assignment
Selecting an appropriate model depends on several factors including assignment requirements and personal preference. Consider these aspects when deciding which framework to use.
- Academic requirements: Check your course syllabus or rubric to see if your instructor requires a specific reflective model or prefers particular elements
- Situation complexity: Simple routine procedures may work well with Driscoll’s model, while ethical dilemmas benefit from Johns’ comprehensive approach
- Personal learning style: Visual learners often prefer Gibbs’ cycle diagram, while analytical thinkers may gravitate toward Kolb’s theoretical framework
- Time and word count: Shorter reflections work better with streamlined models, whereas in-depth analyses require more comprehensive structures
Struggling with Nursing Reflections? Invest in your transcript with StudentResearch.net’s custom papers designed to meet and exceed rubric requirements. Our expert writers transform B- assignments into A+ submissions, ensuring your reflections demonstrate critical thinking and clinical excellence every time
Clinical Experience Reflection Examples for Nursing Students
Clinical experiences form the cornerstone of nursing education, providing opportunities to apply theoretical knowledge in real-world patient care settings. Reflecting on these encounters helps you identify patterns in your practice, recognize areas of strength, and pinpoint opportunities for improvement. The following examples demonstrate how to analyze different types of clinical situations using reflective frameworks. Each example illustrates complete reflection cycles from initial description through final action planning.
Patient Care Reflection Example: First Medication Administration
Your first independent medication administration represents a milestone moment requiring careful reflection on safety protocols and patient interaction. This example uses Gibbs’ Reflective Cycle to analyze the experience systematically.
Situation Description
- Clinical context: Medical-surgical unit during morning medication rounds with a 68-year-old patient recovering from hip replacement surgery
- Your role and preparation: Performed the five rights of medication administration, verified patient identity using two identifiers, and explained the purpose of each medication
- Medications administered: Oral pain medication, anticoagulant, and antibiotic with appropriate timing and documentation
Reflection Analysis
- Emotional journey: Initial nervousness about making errors gradually shifted to confidence after successful completion and positive patient feedback
- Successful elements: Thoroughly checked medication orders against MAR, properly educated patient about side effects, and maintained sterile technique throughout
- Areas for improvement: Rushed through patient education due to anxiety, could have spent more time assessing pain level before and after medication
- Theory application: Applied pharmacology knowledge about drug interactions, contraindications, and therapeutic effects learned in coursework
- Safety considerations: Verified allergy history, checked patient’s renal function before administering medications requiring kidney clearance
- Future action plan: Practice patient education scripts, review common drug interactions, and request supervision for complex medication regimens
Communication Skills Reflection Example: Difficult Patient Interaction
Therapeutic communication challenges provide rich learning opportunities for developing interpersonal skills essential to nursing practice. This reflection examines a conversation with an anxious family member using Driscoll’s model.
Scenario Overview
- What happened: Family member became verbally aggressive when questioning why their loved one hadn’t received pain medication immediately upon request
- Communication barriers: High emotions, cultural expectations about healthcare delivery, and misunderstanding about controlled substance protocols
- Your initial response: Felt defensive and overwhelmed, struggled to maintain professional composure while explaining medication administration policies
Learning Outcomes
- Therapeutic techniques applied: Used active listening, validated family concerns, maintained calm tone despite raised voices, and involved charge nurse appropriately
- Cultural competency demonstrated: Recognized that cultural background influenced expectations about immediate care response and family involvement in decisions
- Professional boundaries: Successfully separated personal feelings from professional responsibility, didn’t take aggressive comments personally
- Communication gaps identified: Need to improve de-escalation techniques, learn to explain policies more clearly under pressure
- Future strategies: Role-play difficult conversations with peers, research cultural communication preferences, develop stock phrases for high-stress interactions
Teamwork Reflection Example: Interdisciplinary Collaboration
Effective healthcare requires seamless collaboration among diverse professionals working toward common patient goals. This brief reflection analyzes your role within the healthcare team.
Team Dynamics Analysis
- Collaboration scenario: Participated in morning rounds with physicians, physical therapists, social workers, and dietitians for discharge planning
- Nursing contributions: Provided updates on patient’s overnight status, mobility progress, medication tolerance, and family concerns about home care
- Leadership observations: Witnessed effective delegation when charge nurse assigned tasks based on each team member’s expertise and scope of practice
Professional Growth Insights
- Effective teamwork strategies: Clear communication using SBAR format, respectful listening to all disciplines’ input, and timely documentation of team decisions
- Improvement opportunities: Need to speak up more confidently during rounds, better understand other disciplines’ roles, and anticipate questions physicians might ask
- Future development goals: Shadow other healthcare professionals to understand their perspectives, practice presenting patient information concisely
Nursing Skills and Procedures Reflection Examples
Technical competency forms the foundation of safe nursing practice, requiring deliberate practice and thoughtful reflection on performance. Each procedure you perform offers opportunities to refine your technique, build confidence, and identify learning needs. These examples show how to reflect on both routine skills and complex clinical judgments. Honest self-assessment of technical abilities protects patient safety and guides your professional development trajectory.
Technical Skills Reflection: Mastering Clinical Procedures
Hands-on procedural skills require repetition and reflection to achieve mastery and maintain patient safety standards. This example examines wound care using Kolb’s learning cycle.
Procedure Example: Wound Care or Catheterization
- Concrete experience: Performed sterile dressing change on post-operative abdominal wound with moderate drainage, required assistance maintaining sterile field
- Patient preparation: Explained procedure to reduce anxiety, positioned patient for optimal access, ensured privacy with curtains, administered pain medication 30 minutes prior
- Infection control protocols: Used strict aseptic technique, properly donned sterile gloves, disposed of contaminated materials in biohazard containers
Competency Development
- Confidence progression: Started nervous about contaminating sterile field, grew more comfortable with each step, ended feeling capable of independent performance next time
- Supervisor feedback received: Preceptor praised thorough hand hygiene and patient communication but noted need to organize supplies before beginning procedure
- Patient comfort considerations: Patient reported minimal discomfort, appreciated gentle technique and clear explanations throughout procedure
- Skill gaps identified: Need more practice with tape application for secure dressing placement, require faster assessment of wound healing stages
- Standards alignment: Reviewed facility wound care policy, compared technique to evidence-based guidelines from wound care nursing specialty organization
- Practice commitment: Will observe three more dressing changes, review wound assessment videos, and practice tape application techniques during lab time
Critical Thinking Reflection Example: Clinical Judgment in Action
Rapid clinical judgment distinguishes experienced nurses from novices and requires reflection to strengthen diagnostic reasoning. This example analyzes recognizing patient deterioration.
Emergency Recognition Scenario
- Warning signs observed: Patient’s oxygen saturation dropped from 95% to 88%, respiratory rate increased to 28 breaths per minute, appeared increasingly anxious and restless
- Time-sensitive decisions: Immediately elevated head of bed, applied supplemental oxygen, and notified charge nurse rather than waiting for scheduled vitals check
- Assessment framework utilized: Performed systematic head-to-toe assessment focusing on respiratory system, auscultated adventitious breath sounds bilaterally
Clinical Reasoning Development
- Theory guiding judgment: Recognized signs of respiratory distress from pathophysiology coursework on gas exchange impairment and hypoxia symptoms
- Collaboration and escalation: Appropriately involved senior nurse who contacted physician, learned when to act independently versus seek guidance
- Prioritization skills: Understood ABCs framework placing airway and breathing above other routine tasks on assignment sheet
- Clinical intuition lessons: Learned to trust “something isn’t right” feeling even when vital signs haven’t drastically changed yet
- Reasoning improvement plan: Will study early warning score systems, practice differentiating urgent from non-urgent changes, shadow experienced nurses during rapid responses
- Evidence integration: Plans to review current research on recognizing clinical deterioration and early intervention protocols
Reflection Due at Midnight? StudentResearch.net’s global writer network and 24/7 support are built for nursing student emergencies. Deadline in 6 hours? No problem. Our healthcare writing specialists deliver high-quality reflections fast, ensuring you never miss a clinical assignment submission again.
Professional Development Reflection Examples for Nursing Students
Professional growth extends beyond technical skills to encompass ethical reasoning, emotional intelligence, and personal wellness practices. These softer aspects of nursing often prove most challenging yet most crucial for long-term career success. Reflecting on ethical dilemmas and self-care needs develops the wisdom and resilience required for sustainable practice. The following examples demonstrate how to process complex professional situations that don’t have clear-cut answers.
Ethical Dilemma Reflection: Navigating Complex Moral Situations
Ethical challenges test your values and require careful consideration of competing principles and stakeholder perspectives. This reflection examines a situation involving patient autonomy.
Ethical Challenge Description
- Dilemma encountered: Competent elderly patient refused recommended medication despite family’s insistence that patient take it, creating tension between autonomy and beneficence
- Autonomy versus safety: Patient had legal right to refuse treatment, yet family worried refusal would lead to preventable complications and suffering
- Your emotional response: Felt torn between respecting patient wishes and acknowledging family’s genuine concern for their loved one’s wellbeing
Ethical Decision-Making Process
- Code of ethics application: Consulted ANA Code of Ethics provisions on patient self-determination, advocacy, and collaboration with families
- Moral distress processing: Discussed conflicting feelings with clinical instructor, recognized that discomfort signals need for ethical reflection rather than wrong action
- Ethics consultation: Charge nurse facilitated family meeting where patient explained reasoning, leading to compromise everyone could accept
- Resolution and learning: Supported patient’s informed decision while ensuring family understood patient’s perspective and legal rights
- Future framework: Will approach similar situations by clarifying each party’s concerns, exploring compromises, and involving ethics committee when needed
Need Discreet Academic Support? Your secret is safe with StudentResearch.net. We employ military-grade encryption and strict confidentiality policies, ensuring your information and service usage remain 100% private. Trust our decade of experience helping nursing students succeed without compromising your academic reputation.
Self-Care and Burnout Prevention Reflection Example
Maintaining personal wellness directly impacts your ability to provide quality patient care and sustain a nursing career. This reflection addresses stress management during demanding rotations.
Recognizing Personal Wellness Needs
- Stress indicators noticed: Difficulty sleeping before clinical days, irritability with classmates, crying after shifts, and physical exhaustion despite adequate rest
- Burnout warning signs: Decreased empathy toward patients, cynicism about healthcare system, and questioning whether nursing was the right career choice
- Impact on performance: Made minor charting errors, struggled to focus during patient interactions, and felt emotionally detached from patient suffering
Building Resilience Strategies
- Self-care implementation: Established non-negotiable sleep schedule, resumed exercise routine three times weekly, set boundaries by not checking school emails after 8 PM
- Work-life balance adjustments: Scheduled enjoyable activities with non-nursing friends, limited talking about clinical experiences outside designated debrief times
- Professional resources accessed: Met with school counselor for stress management strategies, joined peer support group for nursing students
- Mindfulness practices: Started five-minute meditation before clinical shifts, practiced deep breathing during stressful moments, kept gratitude journal
- Support system strengthened: Regular check-ins with mentor, honest conversations with family about challenges, connected with classmates experiencing similar struggles
- Ongoing commitment: Recognized self-care as professional responsibility rather than luxury, developed early warning system for identifying stress escalation
Transform Your Nursing Practice Through Reflection
Reflective practice serves as the bridge between novice uncertainty and expert confidence throughout your nursing journey. When you explore nursing student reflection examples for clinical practice, you’re learning a lifelong skill that separates competent practitioners from truly exceptional nurses. These examples demonstrate that reflection isn’t merely an academic exercise but a fundamental tool for continuous improvement, patient safety, and professional satisfaction.
The nursing student reflection examples presented here illustrate how to systematically analyze diverse situations from medication administration to ethical dilemmas. Learning to write effective reflections with real examples and proven models transforms routine experiences into profound learning opportunities. Each framework—whether Gibbs, Kolb, Johns, or Driscoll—offers a structured approach to extracting maximum insight from your clinical encounters.
Start incorporating regular reflection into your practice immediately after clinical shifts while details remain fresh. Use these nursing student reflection examples as templates, adapting them to your unique experiences and learning style. Remember that honest, thorough reflection directly correlates with enhanced clinical judgment, stronger patient relationships, and increased professional resilience. The investment you make in reflective practice today will compound throughout your entire nursing career, ultimately making you the kind of nurse who positively impacts every patient encounter. Quality reflection transforms good nurses into excellent nurses who continuously evolve and improve.