Table of Contents
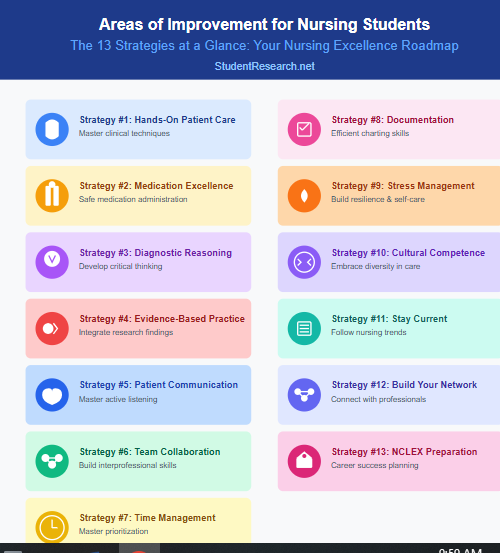
ToggleNursing education demands dedication, resilience, and a commitment to continuous growth. As you navigate through clinical rotations, coursework, and practical assessments, identifying and addressing your areas of improvement for nursing students becomes essential for success. Student research consistently shows that students who actively work on their weaknesses while building on their strengths achieve better clinical outcomes and greater confidence in patient care. This comprehensive guide explores 13 evidence-based strategies that will help you excel in your nursing education and prepare for a rewarding healthcare career.
How to Improve Clinical Skills and Technical Competencies
Clinical competency forms the foundation of excellent nursing practice. These hands-on skills directly impact patient safety, treatment outcomes, and your confidence in clinical settings. Mastering technical competencies early in your education creates a solid platform for advanced practice and specialization.
Ways to Refine Hands-On Patient Care Techniques
Practice venipuncture and IV insertion systematically by utilizing every opportunity in simulation labs. Request feedback from clinical instructors on your technique, angle of insertion, and patient communication during procedures. Repetition builds muscle memory and confidence.
Master wound care and dressing changes through deliberate practice sessions. Learn to assess wound healing stages, select appropriate dressing materials, and document changes accurately. Understanding the rationale behind each step improves your clinical judgment.
Build confidence through simulation labs and peer practice by scheduling extra time with manikins and simulation equipment. Practice scenarios with classmates, alternating between patient and nurse roles. This collaborative approach reveals different techniques and problem-solving strategies.
Steps to Achieve Medication Administration Excellence
Medication administration represents one of the most critical responsibilities in nursing practice, requiring meticulous attention to detail, comprehensive pharmacological knowledge, and unwavering commitment to patient safety. Follow these essential steps to achieve excellence:
Step 1: Verify the complete medication order by checking the physician’s prescription against the medication administration record (MAR). Ensure all components are present including drug name, dose, route, frequency, and any special instructions.
Step 2: Perform the three checks systematically by verifying the medication label when removing it from storage, when preparing the dose, and immediately before administration. This triple-check system catches errors before they reach the patient.
Step 3: Calculate dosages accurately using dimensional analysis or ratio-proportion methods, and always have a colleague verify complex calculations. Never guess or estimate medication doses, especially for high-alert medications.
Step 4: Assess the patient before administration by checking vital signs, reviewing lab values, and evaluating for contraindications. Certain medications require specific assessments like checking heart rate before digoxin or blood pressure before antihypertensives.
Step 5: Use two patient identifiers by asking the patient to state their full name and date of birth while comparing this information with the patient’s wristband and MAR. Never skip this step even with familiar patients.
Step 6: Educate the patient about the medication by explaining its purpose, expected effects, and potential side effects. This empowers patients to participate in their care and report concerns promptly.
Step 7: Administer medications using proper technique whether oral, injectable, topical, or intravenous. Follow evidence-based guidelines for each route and maintain sterile technique when required.
Step 8: Monitor for immediate reactions by staying with the patient for several minutes after administration, especially with first doses, IV medications, or known allergens. Watch for signs of adverse reactions.
Step 9: Document administration immediately including the medication name, dose, route, site (for injections), time given, and patient response. Never document before actually administering the medication.
Step 10: Evaluate medication effectiveness by reassessing the patient after appropriate intervals. For pain medications, reassess within 30-60 minutes; for antihypertensives, check blood pressure according to facility protocol.
Understanding Pharmacology: Essential Areas of Improvement
Deep dive into drug classifications and mechanisms by creating personal study guides that connect drug actions to pathophysiology. Understanding why medications work helps you anticipate side effects and patient responses, making you a safer practitioner.
Implement the “five rights” consistently in every medication administration scenario: right patient, right medication, right dose, right route, and right time. Develop personal checklists and never skip steps, even in simulation settings where consequences seem minimal.
How to Recognize Adverse Drug Reactions
Identify early warning signs by studying common adverse reactions for frequently administered medications. Learn to distinguish between expected side effects and serious adverse reactions requiring immediate intervention.
Master documentation and reporting protocols by practicing thorough, timely charting of medication administration and patient responses. Understand your facility’s chain of command for reporting concerns and never hesitate to escalate when patient safety is at risk.
Critical Thinking and Clinical Judgment: Key Areas of Improvement for Nursing Students
Critical thinking separates adequate nurses from exceptional ones. The ability to analyze complex situations, synthesize information, and make sound clinical judgments develops through intentional practice and reflection. These cognitive skills become automatic with consistent application in diverse patient scenarios.
How to Develop Diagnostic Reasoning Skills
Learn to prioritize patient needs using clinical frameworks such as Maslow’s hierarchy or the ABC (airway, breathing, circulation) approach. Practice ranking patient concerns during post-conference discussions and compare your reasoning with experienced nurses.
Identify subtle changes in patient conditions by establishing baseline assessments and monitoring trends rather than isolated values. Develop your clinical intuition by asking yourself “what could this mean?” when you notice variations from normal.
Benefits of Evidence-Based Decision Making
Improve patient outcomes and safety by basing clinical decisions on the most current, high-quality research rather than tradition or anecdotal experience alone.
Increase confidence in your clinical judgment as you support your nursing interventions with solid evidence, making you a more credible and effective advocate for patients.
Reduce medical errors and complications by implementing proven protocols that have demonstrated effectiveness across diverse patient populations and clinical settings.
Enhance professional credibility among healthcare team members who recognize and value your commitment to evidence-based practice and continuous quality improvement.
Stay current with evolving healthcare standards by regularly reviewing new research findings and translating them into practical bedside applications.
Contribute to better resource utilization by identifying which interventions provide the best outcomes, eliminating wasteful or outdated practices that don’t benefit patients.
Need Help with Nursing Assignments? We Do It All!
StudentResearch.net offers comprehensive academic support including research papers, case studies, care plans, essays, dissertations, presentations, literature reviews, and professional editing services. Expert writers with nursing backgrounds deliver excellence across all assignment types. Your one-stop academic solution.
Ways to Integrate Research into Practice
Access and evaluate nursing literature through your school’s database subscriptions. Learn to read research articles critically, distinguishing between strong evidence and preliminary findings. Join journal clubs to discuss current research with peers.
Apply evidence to patient scenarios by questioning “what does the research say?” when faced with clinical decisions. Bridge the gap between theoretical knowledge and practical application by relating journal findings to your patient assignments.
When to Question Outdated Protocols
Develop professional advocacy strategies by learning how to present evidence-based alternatives respectfully. Approach experienced nurses with curiosity rather than criticism, asking questions like “I read about a different approach—what’s your experience with that?”
Use a collaborative approach to protocol updates by understanding institutional review processes. Participate in quality improvement initiatives and contribute to evidence-based practice councils when opportunities arise.
Guide to Communication and Interprofessional Collaboration
Effective communication prevents errors, builds trust, and ensures coordinated patient care. Strong interprofessional skills distinguish competent nurses from exceptional team members. Communication competency directly impacts patient satisfaction, safety outcomes, and professional relationships.
Types of Patient Communication Mastery
Therapeutic communication builds trust through empathy, active listening, and non-judgmental responses that encourage patients to share concerns openly.
Clear health education translates complex medical information into understandable language that empowers patients to make informed decisions.
Non-verbal communication awareness involves recognizing and appropriately responding to body language, facial expressions, and cultural communication differences.
Assertive communication enables you to advocate for patient needs while maintaining professional boundaries and collaborative relationships.
How to Practice Active Listening Techniques
Use open-ended questions effectively by replacing yes/no questions with prompts like “Tell me about your pain” or “What concerns you most about this procedure?” This approach reveals information patients might not volunteer spontaneously.
Read and respond to non-verbal cues by observing body language, facial expressions, and tone of voice. Recognize when verbal and non-verbal messages don’t align, and gently explore these discrepancies with empathetic follow-up questions.
Steps to Adapt Health Literacy: Critical Areas of Improvement
Explain medical terms in plain language by avoiding jargon and acronyms. Instead of saying “you’re experiencing dyspnea,” say “you’re having difficulty breathing.” Check yourself constantly for healthcare language that patients may not understand.
Check patient understanding through teach-back methods by asking patients to explain information in their own words. Rather than “Do you understand?” ask “Can you show me how you’ll take this medication at home?” This reveals comprehension gaps requiring clarification.
Ways to Build Team Collaboration Skills
Practice effective interprofessional communication using standardized tools like SBAR to convey patient information clearly and concisely to all team members.
Demonstrate respect for all disciplines by acknowledging each healthcare professional’s unique expertise and contributions to comprehensive patient care.
Participate actively in team rounds and huddles by coming prepared with relevant patient updates and thoughtfully contributing to care planning discussions.
Develop conflict resolution skills to address disagreements professionally while maintaining focus on patient-centered outcomes and team cohesion.
Seek opportunities for collaborative learning through interdisciplinary case studies, simulation exercises, and shadowing experiences with various healthcare professionals.
Understanding SBAR Communication
Master the Situation, Background, Assessment, Recommendation framework for concise, organized communication with physicians and team members. This structured approach ensures you include all essential information without overwhelming the listener.
Know when to use SBAR in clinical settings including shift handoffs, calling physicians about patient concerns, and emergency situations. Practice SBAR communication in simulation scenarios until it becomes second nature.
How to Build Rapport with Healthcare Teams
Practice interprofessional etiquette and respect by acknowledging the expertise each team member brings to patient care. Avoid hierarchical thinking and recognize that respiratory therapists, physical therapists, and social workers possess specialized knowledge you lack.
Contribute meaningfully to team discussions by preparing relevant patient information before rounds. Speak up with observations and concerns while remaining open to other perspectives and alternative solutions.
Time Management and Organization Strategies
Efficient time management prevents medication errors, ensures timely interventions, and reduces stress in clinical settings. Organizational skills allow you to provide safe care for multiple patients simultaneously. These competencies develop through systematic practice and continuous refinement of personal systems.
How to Master Prioritization in Clinical Settings
Assess all patients systematically at shift start to identify immediate needs, potential complications, and time-sensitive interventions requiring urgent attention.
Use the ABC framework (airway, breathing, circulation) to quickly determine which patients need immediate intervention versus those who can wait safely.
Create and maintain organized task lists that categorize activities by urgency and importance, updating them throughout your shift as conditions change.
Communicate priorities with your team by delegating appropriate tasks and alerting colleagues when you need assistance with competing demands.
Understanding Urgency vs Importance: Areas of Improvement
| Urgent & Important | Not Urgent but Important |
| Active chest pain or respiratory distress | Patient education before discharge |
| Severe bleeding or trauma | Updating care plans |
| Critical lab values | Routine assessments |
| Medication errors requiring intervention | Documentation completion |
| Cardiac arrest or code situations | Professional development activities |
Use priority matrices for patient care by categorizing tasks into urgent/important quadrants. Address urgent and important tasks immediately, schedule important but non-urgent tasks, and delegate or defer less critical activities when appropriate.
Manage multiple patient assignments safely by creating visual organization systems like brain sheets or personalized worksheets. Cluster care activities to maximize efficiency while ensuring you don’t miss critical assessments or time-sensitive medications.
Examples of Effective Clinical Prioritization
Apply real-world scenarios and decision trees by mentally rehearsing “what if” situations. When assigned multiple patients, determine who needs immediate assessment versus who can wait 15 minutes while you address urgent needs.
Master responding to emergencies while maintaining routine care by staying calm and systematically delegating when possible. Communicate with team members about delayed routine tasks and catch up as soon as the emergency stabilizes.
Steps to Documentation Efficiency
Chart accurately and promptly without sacrificing quality by documenting throughout your shift rather than leaving everything until the end. Use downtime between patient activities to complete charting while details remain fresh.
Utilize electronic health records effectively by learning keyboard shortcuts, templates, and smart phrases that speed documentation. Attend EHR training sessions and practice navigating the system during simulation time.
Implement time-saving documentation strategies like charting by exception for normal findings while thoroughly documenting abnormal assessments, interventions, and patient responses. Always prioritize accuracy over speed.
Emotional Intelligence and Self-Care: Essential Areas of Improvement for Nursing Students
Emotional intelligence enables therapeutic relationships, professional resilience, and sustained career satisfaction. Self-care prevents burnout and maintains the physical and mental stamina nursing demands. Recognizing these as essential professional skills rather than optional extras transforms your approach to nursing education.
How to Manage Stress and Prevent Burnout
Develop a consistent self-care routine including regular exercise, adequate sleep (7-9 hours), nutritious meals, and activities that bring you joy outside of nursing.
Practice stress-reduction techniques daily such as deep breathing exercises, meditation, progressive muscle relaxation, or mindfulness to manage acute stress responses.
Establish healthy boundaries by learning to say no to excessive commitments and protecting personal time for rest and recovery.
Build a strong support network of peers, mentors, family, and friends who understand nursing challenges and provide emotional support.
Recognize your stress triggers early by monitoring physical symptoms like headaches, fatigue, irritability, or sleep disturbances that signal approaching burnout.
Seek professional help when needed through counseling services, employee assistance programs, or mental health professionals specializing in healthcare worker wellness.
Your Secret to Academic Success, Safely Guarded
Worried about privacy? StudentResearch.net guarantees complete confidentiality with military-grade encryption, secure payment systems, and strict data protection policies. Your personal information and orders remain 100% private—always. Trust us with your academic success confidentially.
Ways to Build Resilience: Critical Areas of Improvement
Develop healthy coping mechanisms including regular exercise, adequate sleep, and stress-reduction techniques like meditation or deep breathing. Identify your personal stress signals and intervene before reaching crisis points.
Recognize signs of compassion fatigue early including emotional numbness, cynicism about patients, or dreading clinical days. Seek support from counselors, mentors, or peer support groups when these symptoms emerge.
Understanding Work-Life Balance Importance
Set boundaries during clinical rotations by protecting time for rest, relationships, and activities unrelated to nursing. Learn to say no to extra shifts or volunteer opportunities when your schedule is already overwhelming.
Understand why self-care is not selfish in nursing but rather an ethical obligation. Exhausted, stressed nurses make errors and provide suboptimal care. Taking care of yourself ensures you can properly care for patients.
What is Cultural Competence and Why It Matters
Cultural competence is the ability to understand, appreciate, and effectively interact with people from diverse cultural backgrounds, beliefs, and practices. It involves recognizing your own cultural biases while respecting patients’ unique values, traditions, and healthcare preferences to provide individualized, patient-centered care.
Improves patient trust and therapeutic relationships by demonstrating respect for cultural values, beliefs, and healthcare practices that differ from your own.
Enhances treatment adherence and outcomes when patients feel understood and care plans incorporate their cultural preferences and traditions.
Reduces health disparities by identifying and addressing barriers that prevent certain populations from receiving equitable, quality healthcare.
Prevents miscommunication and errors that arise from cultural misunderstandings about symptoms, medication use, or treatment expectations.
Fulfills ethical and legal obligations to provide non-discriminatory care that respects patient autonomy and dignity regardless of background.
Steps to Understanding Diverse Patient Backgrounds
Practice cultural humility by approaching each patient as an individual expert on their own cultural needs and preferences. Avoid stereotypes while acknowledging that cultural backgrounds influence health beliefs and practices.
Address implicit biases through self-reflection and education about diverse populations. Complete implicit bias training modules and honestly examine how your assumptions might affect patient care decisions.
How to Provide Compassionate, Patient-Centered Care
Develop individualized care planning that incorporates patient preferences, cultural considerations, and personal goals. Partner with patients in decision-making rather than imposing standardized protocols without discussion.
Respect cultural healthcare practices by learning about traditional healing methods, religious considerations, and family dynamics in different cultures. Integrate complementary approaches when safe and desired by patients.
Professional Development and Lifelong Learning
Nursing science evolves rapidly, requiring commitment to continuous learning throughout your career. Professional development distinguishes nurses who merely maintain licensure from those who drive innovation and excellence. Building these habits during nursing school establishes patterns that serve you throughout your professional life.
Ways to Stay Current with Nursing Trends
Engage with professional journals and publications by subscribing to nursing journals in your areas of interest. Read at least one article weekly and consider how new research applies to your clinical practice.
Attend continuing education opportunities including conferences, webinars, and certification courses. Many organizations offer student rates, making these valuable learning experiences accessible during nursing school.
Follow evidence-based practice updates by subscribing to professional organization newsletters and following thought leaders on professional social media platforms. Staying informed about practice changes prepares you for evolving healthcare environments.
How to Build a Professional Network
Join professional nursing organizations like NSNA, specialty nursing associations, or local chapters that align with your career interests and goals.
Attend nursing conferences and workshops to meet practicing nurses, educators, and healthcare leaders while staying current on industry trends.
Engage on professional social media platforms such as LinkedIn to connect with nursing professionals and participate in meaningful healthcare discussions.
Volunteer at health fairs and community events where you can network with healthcare professionals while serving your community.
Seek informational interviews with nurses working in specialties that interest you to learn about career paths and build mentoring relationships.
H4: Benefits of Joining Student Nursing Organizations
Access mentorship and resources through organizations like the National Student Nurses’ Association (NSNA). These groups provide leadership opportunities, professional development, and connections with practicing nurses in various specialties.
Leverage networking opportunities for career advancement by attending conferences, volunteering at health fairs, and participating in organization initiatives. The relationships you build during nursing school often lead to job opportunities and career guidance.
How to Find Mentors in Your Specialty Area
Identify potential mentors by observing nurses whose practice style, specialty focus, or career path aligns with your goals. Look for approachable professionals who demonstrate teaching skills and genuine interest in student development.
Build meaningful mentor-mentee relationships by clearly communicating your goals and regularly seeking guidance. Respect your mentor’s time by coming prepared with specific questions and demonstrating how you’ve applied their advice.
Steps to NCLEX Preparation and Career Success
Begin NCLEX preparation early in nursing school by consistently reviewing content from each course rather than cramming everything in the final semester before graduation.
Complete practice questions daily using reputable NCLEX review resources like UWorld, Kaplan, or NCLEX-RN review books to familiarize yourself with question formats and testing strategies.
Identify and strengthen weak content areas through targeted study sessions focusing on topics where practice questions reveal knowledge gaps or consistent errors.
Join or create NCLEX study groups with classmates to discuss rationales, share study strategies, and maintain accountability throughout the preparation process.
Take full-length practice exams under timed conditions to build testing endurance and identify time management issues before the actual examination.
Develop a realistic study schedule that balances NCLEX review with clinical responsibilities, coursework, and self-care to prevent burnout during preparation.
Research job opportunities early by attending career fairs, networking with potential employers, and preparing professional resumes and cover letters before graduation.
How to Develop Effective Study Habits: Areas of Improvement
Apply evidence-based study techniques including spaced repetition, practice questions, and teaching concepts to peers. These methods outperform passive reading or cramming for long-term retention and application.
Create personalized study schedules that accommodate your learning style, peak concentration times, and other commitments. Consistency matters more than marathon study sessions—daily practice builds lasting knowledge.
Understanding NCLEX Requirements
Research licensure requirements by state since regulations vary regarding background checks, fees, and application processes. Begin gathering necessary documentation early to avoid delays after graduation.
Master test-taking strategies for success by completing thousands of practice questions and learning to identify question patterns. Understand how NCLEX uses next-generation items and familiarize yourself with various question formats.
How to Create Your Personal Areas of Improvement Action Plan
Taking ownership of your professional development accelerates growth and builds accountability. A personalized improvement plan transforms vague intentions into concrete actions with measurable outcomes. This strategic approach to areas of improvement for nursing students ensures you address weaknesses systematically while building on existing strengths.
Steps to Self-Assessment and Goal Setting
Conduct honest self-evaluations regularly by reflecting on clinical experiences, identifying strengths you can leverage, and recognizing weaknesses requiring improvement.
Review instructor feedback systematically from clinical evaluations, written assignments, and skills assessments to identify recurring themes and patterns.
Compare your performance to program competencies and learning objectives to understand where you meet expectations and where gaps exist.
Set specific, measurable goals with clear timelines and action steps rather than vague aspirations like “get better at nursing.”
Track your progress consistently using journals, skills checklists, or digital tools that document improvements and celebrate achievements along the way.
Ways to Identify Your Personal Areas of Improvement
Use reflective practice journaling techniques by documenting clinical experiences, challenges encountered, and lessons learned. Review entries monthly to identify recurring themes and patterns requiring attention.
Seek feedback from instructors and peers through regular check-ins and post-clinical conferences. Ask specific questions like “What’s one thing I could improve in my patient assessments?” rather than generic “How did I do?”
How to Set SMART Goals for Nursing Growth
Create Specific, Measurable, Achievable, Relevant, Time-bound objectives such as “I will successfully start three IVs with instructor supervision by the end of this clinical rotation” rather than “I want to get better at IVs.”
Track progress and celebrate milestones by maintaining a skills checklist and acknowledging achievements. Recognizing progress, even small victories, maintains motivation through challenging periods of nursing education.
Benefits of Seeking Feedback and Mentorship
Embrace constructive criticism for growth by viewing feedback as valuable information rather than personal attacks. Ask clarifying questions when feedback seems unclear and develop action plans addressing identified concerns.
Work effectively with clinical instructors by communicating openly about learning goals, requesting specific learning experiences, and demonstrating receptiveness to teaching. Strong instructor relationships enhance your educational experience significantly.
Build a support system for success through study groups, peer mentoring arrangements, and professional relationships. Nursing education challenges everyone—you don’t have to navigate it alone.
Conclusion
Mastering these 13 powerful strategies for areas of improvement for nursing students creates a foundation for clinical excellence and professional success. Remember that improvement is a continuous journey, not a destination—even experienced nurses constantly refine their practice through reflection and learning. The most successful nursing students recognize their weaknesses without shame, actively work to address them, and celebrate progress along the way. Choose one strategy from this guide to implement today, whether it’s refining your IV technique, practicing SBAR communication, or establishing better study habits. Excellence in nursing comes from consistent growth, deliberate practice, and unwavering commitment to providing the best possible patient care. Your dedication to continuous improvement will serve your patients, your colleagues, and your career throughout your nursing journey.
Struggling with Your Nursing Budget? We’ve Got You Covered!
StudentResearch.net understands student financial constraints. Enjoy competitive rates, exclusive first-time user discounts, loyalty rewards, and seasonal promotions designed specifically for nursing students. Quality academic writing support that fits your budget—because education shouldn’t break the bank.