Table of Contents
ToggleIt’s the night before your first clinical rotation, and anxiety is keeping you awake. You’re wondering whether you’ll measure up, whether your preceptor will be supportive, and whether you’ll know what to do with real patients. You’re not alone. Student research shows that 78% of NP students report moderate to high anxiety about meeting clinical requirements, making this transition one of the most stressful periods in nurse practitioner education.
The solution? Clinical objectives for nurse practitioner students serve as your roadmap, transforming vague expectations into concrete, achievable goals. These aren’t bureaucratic checkboxes; they’re carefully designed competencies bridging theory and practice. Student research demonstrates that students who actively engage with their objectives from day one report significantly higher confidence, better preceptor relationships, and more successful outcomes.
This guide will show you how to master clinical objectives efficiently. You’ll discover the five core types of objectives, step-by-step strategies for setting rotation-specific goals, seven proven techniques to accelerate progress, and solutions to common problems. By the end, you’ll have a clear action plan to transform anxiety into achievement.
What Are Clinical Objectives for Nurse Practitioner Students: The 5 Core Types You Must Master
Before you can excel in your clinical rotations, you need to understand exactly what you’re working toward. Clinical objectives represent specific, measurable competencies that define what a proficient nurse practitioner must know, do, and demonstrate in real-world healthcare settings. Understanding the five core types of clinical objectives will help you organize your learning, communicate effectively with preceptors, and ensure you’re developing the comprehensive skill set required for independent practice.
Understanding Clinical Objectives: Definition and Why They Matter
Clinical objectives serve as the blueprint for your transformation from student to practicing clinician, providing clear benchmarks that guide your professional development.
- Definition: Clinical objectives are predetermined learning outcomes that specify the knowledge, skills, and attitudes you must demonstrate during supervised clinical practice to achieve competency as a nurse practitioner
- Purpose in NP education: They create accountability for both students and preceptors, ensuring standardized competency development across diverse clinical settings and preventing knowledge gaps that could compromise patient safety
- Difference from academic goals: Unlike classroom objectives focused on theoretical understanding and exam performance, clinical objectives emphasize real-time application, patient interaction, clinical reasoning, and hands-on procedural skills in authentic healthcare environments
- Why they matter for success: Research indicates that students who clearly understand their clinical objectives perform 40% better on competency evaluations, experience less rotation-related stress, and develop stronger professional confidence compared to those with ambiguous expectations
H3: Type #1 – Patient Assessment and Diagnostic Reasoning Objectives
Mastering comprehensive patient assessment forms the foundation of all other clinical competencies, as accurate diagnosis depends entirely on your ability to gather and interpret clinical data.
- What this means in practice: You’ll conduct systematic health histories, perform thorough physical examinations across all body systems, identify abnormal findings, formulate differential diagnoses, and order appropriate diagnostic tests
- Core assessment objectives include:
- Conducting age-appropriate comprehensive and focused health assessments
- Demonstrating proper physical examination techniques for all body systems
- Identifying normal versus abnormal findings with clinical significance
- Developing evidence-based differential diagnoses using clinical reasoning
- Selecting appropriate diagnostic studies and interpreting results accurately
- Why this is foundational: Every clinical decision you make—from prescribing medications to referring patients—depends on accurate assessment; weak assessment skills compromise all subsequent clinical activities and patient outcomes
How to Develop Strong Assessment Skills
- First day strategies: Shadow your preceptor closely during initial assessments, ask permission to observe complete examinations, take detailed notes on technique and sequencing, and request demonstrations of specialized examination maneuvers
- Common mistakes to avoid: Rushing through history-taking to appear efficient, skipping body systems you find uncomfortable examining, failing to verify findings when uncertain, and neglecting to document assessment rationale
- Preceptor-approved techniques: Practice systematic head-to-toe approaches consistently, verbalize your clinical thinking aloud during assessments, prepare patient-specific assessment plans before encounters, and review assessment findings immediately after each patient
Type #2 – Evidence-Based Treatment Planning Objectives
Once you’ve accurately assessed and diagnosed your patient, you must develop comprehensive treatment plans grounded in current evidence and individualized to patient circumstances.
- Breaking down treatment decisions: Effective treatment planning requires integrating clinical guidelines, patient preferences, cost considerations, cultural factors, and potential barriers to adherence into unified care plans
- Pharmacological treatment objectives:
- Selecting appropriate medications based on evidence-based guidelines and patient-specific factors
- Calculating correct dosages and understanding pharmacokinetics across different patient populations
- Recognizing contraindications, drug interactions, and adverse effect profiles
- Providing clear patient education about medication administration, expected outcomes, and side effects
- Non-pharmacological approaches: Lifestyle modifications, behavioral interventions, physical therapy referrals, complementary therapies, and patient education strategies that address root causes
- Real-world application examples: Developing a hypertension management plan that considers a patient’s work schedule for medication timing, recommending dietary modifications aligned with cultural food preferences, or creating diabetes education plans appropriate to health literacy levels
Type #3 – Professional Communication and Collaboration Objectives
Healthcare delivery requires seamless teamwork, making communication competencies essential for patient safety and care coordination.
- Interprofessional teamwork objectives: Effectively collaborating with physicians, specialists, pharmacists, social workers, and other healthcare providers while respecting scope of practice boundaries and maintaining professional relationships
- Documentation competency targets:
- Creating thorough, accurate, legally defensible medical records
- Using appropriate medical terminology and professional language
- Documenting clinical reasoning and decision-making processes
- Meeting billing and coding requirements accurately
- Completing documentation in timely manner per institutional policies
- Patient education goals: Translating complex medical information into understandable terms, assessing patient comprehension through teach-back methods, creating culturally sensitive education materials, and empowering patients in shared decision-making
Type #4 – Ethical and Legal Practice Objectives
Every clinical decision carries ethical and legal implications that protect both patients and your professional license.
- Key ethical objectives for rotations: Obtaining proper informed consent, maintaining patient confidentiality, recognizing situations requiring ethics consultation, navigating end-of-life care decisions, and addressing social determinants of health
- Legal compliance goals: Understanding scope of practice limitations, following appropriate prescribing regulations, implementing proper documentation for legal protection, recognizing mandatory reporting requirements, and maintaining professional liability awareness
- Risk management awareness: Identifying high-risk situations, implementing appropriate follow-up systems, recognizing when to seek consultation, and understanding how to respond when medical errors occur
Type #5 – Self-Directed Learning and Professional Growth Objectives
Your ability to identify knowledge gaps and independently pursue learning opportunities determines your long-term success beyond graduation.
- Building clinical confidence objectives: Progressively increasing autonomy in patient care, developing clinical intuition through pattern recognition, learning to trust your clinical judgment while maintaining appropriate caution, and cultivating professional identity
- Feedback utilization goals: Actively seeking constructive criticism, implementing feedback into practice improvements, engaging in regular self-reflection about clinical performance, and maintaining learning portfolios that track growth over time
- Lifelong learning competencies: Staying current with evolving evidence through regular literature review, participating in professional development opportunities, engaging with professional organizations, and maintaining certification requirements throughout your career
How to Set Clinical Objectives for Nurse Practitioner Students: Step-by-Step Guide by Rotation
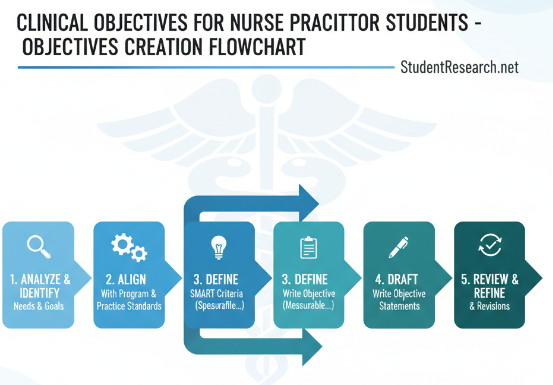
Setting effective clinical objectives isn’t one-size-fits-all; your goals must evolve as you progress through different rotation types and specialty areas. This section provides a systematic approach to creating objectives that match your developmental stage, clinical setting, and specialty focus, ensuring continuous growth from your first nervous day through your final confident rotation.
Steps to Create Your First Rotation Clinical Objectives
Your inaugural clinical rotation sets the foundation for everything that follows, making it crucial to establish realistic, achievable objectives that build confidence rather than overwhelm you.
- Week-by-week progression framework: Break your rotation into distinct phases with escalating expectations—observation and integration in weeks 1-2, supervised practice in weeks 3-5, and increasing autonomy in weeks 6-8
- Setting realistic expectations: Expect to feel uncomfortable initially; competence develops gradually through repeated exposure, and perfectionism sabotages learning by creating paralyzing anxiety
- SMART objectives for beginners:
- Specific: “Conduct complete cardiovascular assessments on 5 patients” rather than “improve assessment skills”
- Measurable: “Document 10 comprehensive SOAP notes reviewed by preceptor” instead of “work on documentation”
- Achievable: “Formulate differential diagnoses for common complaints” not “diagnose all conditions independently”
- Relevant: Align with your rotation specialty and program competencies
- Time-bound: “By week 4” or “within first month” to create accountability
How to Set Week 1-2 Objectives: Building Your Foundation
- Observation and integration goals:
- Shadow preceptor for complete patient encounters to understand clinic workflow
- Observe at least 15-20 diverse patient presentations
- Learn electronic health record navigation and documentation templates
- Identify appropriate times to ask questions without disrupting patient care
- Building rapport with preceptors:
- Communicate your learning style and previous clinical experience honestly
- Ask about preceptor’s preferred teaching methods and feedback style
- Demonstrate reliability by arriving early, staying engaged, and following through
- Express gratitude for teaching time and acknowledge preceptor expertise
- Documentation practice targets:
- Complete 3-5 practice notes on observed patients for preceptor review
- Learn billing codes and documentation requirements specific to the setting
- Understand which elements require preceptor co-signature
Setting Week 3-8 Objectives: Advancing Your Skills
- Increasing patient load targets: Progress from 2-3 patients daily to 5-8 by rotation end, adjusting based on patient complexity and setting expectations
- Diagnostic reasoning development goals:
- Present cases to preceptor using organized problem-based format
- Generate differential diagnoses before discussing with preceptor
- Defend clinical reasoning with evidence from history, exam, and literature
- Independent practice preparation:
- Develop complete treatment plans before preceptor input
- Practice patient education and counseling with decreasing supervision
- Perform procedures with preceptor observation rather than assistance
How to Adapt Clinical Objectives for Mid-Program Specialty Rotations
As you advance through your program, objectives must shift from basic skill acquisition to specialty-specific competency and sophisticated clinical reasoning.
- Adjusting to different clinical settings: Urgent care requires rapid assessment and decision-making objectives, while primary care emphasizes continuity and prevention goals; acute hospital settings prioritize complex diagnostic reasoning and critical care management objectives
- Understanding setting-specific expectations:
- Outpatient clinics: Focus on chronic disease management, preventive care, and longitudinal patient relationships
- Emergency departments: Emphasize rapid triage, acute symptom management, and appropriate disposition decisions
- Specialty practices: Develop depth in specific body systems, advanced procedures, and complex condition management
- Tracking diverse patient encounters: Most programs require specific numbers across demographics (age, gender, diagnoses), so strategically pursue gaps in your clinical log early in rotations
Examples of Specialty-Specific Clinical Objectives
- Pediatrics clinical objectives:
- Conduct age-appropriate developmental assessments for infants through adolescents
- Master pediatric immunization schedules and catch-up protocols
- Demonstrate effective communication with both children and parents
- Perform pediatric physical exam modifications including growth measurements
- Women’s health clinical objectives:
- Complete comprehensive gynecological examinations and pap smears
- Provide contraceptive counseling across diverse methods
- Manage common conditions like UTIs, yeast infections, and menstrual disorders
- Conduct prenatal visits and understand normal pregnancy progression
- Acute care clinical objectives:
- Interpret diagnostic studies including labs, ECGs, and imaging rapidly
- Manage patients with multiple comorbidities and complex medication regimens
- Collaborate with interdisciplinary teams during rounds and care transitions
- Develop appropriate discharge planning and follow-up coordination
- Psychiatric mental health clinical objectives:
- Conduct comprehensive mental status examinations
- Demonstrate therapeutic communication and de-escalation techniques
- Prescribe and manage psychotropic medications safely
- Assess suicide and violence risk systematically
Guide to Setting Final Rotation Objectives: Preparing for Independent Practice
Your final rotations represent the transition from supervised student to autonomous practitioner, requiring objectives that demonstrate readiness for independent clinical decision-making.
- Demonstrating autonomous practice readiness: Function as independently as legally permitted with minimal preceptor intervention, manage your own patient panel with appropriate consultation, and handle unexpected situations confidently while knowing when to seek guidance
- Certification exam preparation through objectives:
- Deliberately seek patient presentations matching certification exam content outlines
- Practice comprehensive documentation that mirrors exam case study formats
- Review clinical guidelines for common conditions you’ll encounter on exams
- Discuss complex cases using evidence-based reasoning required for certification
- Job readiness skill objectives:
- Practice time management with realistic patient volumes for employment settings
- Understand billing, coding, and productivity expectations
- Develop systematic approaches to common chief complaints
- Build confidence in independent prescribing and procedure performance
- Establish professional boundaries and self-care practices for sustainable practice
7 Proven Ways to Achieve Clinical Objectives for Nurse Practitioner Students Faster
Knowing your objectives is only half the battle; implementing proven strategies accelerates your progress and maximizes limited rotation time. These seven evidence-based approaches help you achieve competency more efficiently while reducing stress and building confidence throughout your clinical experiences.
Strategy #1 – How to Create a Weekly Clinical Preparation Routine
Consistent preparation transforms good students into exceptional clinicians by ensuring you arrive at each rotation ready to maximize learning opportunities.
- Pre-rotation research checklist:
- Review your rotation-specific objectives the night before each clinical day
- Research common conditions and chief complaints for your scheduled patient population
- Prepare questions to ask your preceptor about challenging concepts
- Review any procedures you might observe or perform the following day
- Refresh clinical guidelines relevant to your rotation specialty
- Evidence-based resources to use:
- UpToDate for current clinical management guidelines and drug information
- CDC and USPSTF websites for preventive care and immunization recommendations
- Specialty-specific guidelines from professional organizations (AHA, ADA, ACOG)
- Mobile apps like Epocrates, Medscape, or Calculate for point-of-care decision support
- Time management templates: Allocate 30-45 minutes nightly for clinical prep, 2-3 hours weekly for comprehensive case reviews, and 1 hour monthly for objective progress assessment and adjustment
Struggling to Structure Your Clinical Papers? StudentResearch.net delivers custom academic papers as expert study guides. It’s not cheating—it’s strategic learning. Master proper structure, citation formats, and clinical argumentation with professionally crafted examples tailored to your assignment requirements
Strategy #2 – How to Master Clinical Documentation for Your Objectives
Excellent documentation not only meets legal and billing requirements but also demonstrates your clinical reasoning and objective achievement to preceptors and program faculty.
- Templates that improve quality:
- Create personalized SOAP note templates with prompts for all required elements
- Develop specialty-specific templates (well-child checks, chronic disease visits, acute complaints)
- Include objective-specific sections to document competency demonstration
- Use standardized phrases for common scenarios while maintaining personalization
- Common documentation errors to avoid:
- Copying forward previous notes without updating current assessment and status
- Using ambiguous terms like “within normal limits” without documenting actual findings
- Failing to document medical decision-making rationale and risk considerations
- Omitting patient education, instructions, and follow-up plans
- Missing required billing elements or using inappropriate codes
- Using objectives to guide documentation: Reference specific objectives achieved in each encounter, document progressive skill development, include preceptor observations of competency, and maintain portfolio examples demonstrating objective mastery
Strategy #3 – Ways to Build Strong Preceptor Relationships
Your preceptor relationship profoundly impacts learning quality, reference letters, and future networking opportunities, making this relationship your most valuable clinical asset.
- First impression strategies: Dress professionally, arrive 15 minutes early, bring required documentation and equipment, demonstrate genuine enthusiasm, silence your phone, and avoid complaining about your program or previous rotations
- How to ask for feedback effectively:
- Request specific feedback on particular skills rather than general impressions
- Ask “What should I focus on improving this week?” versus “How am I doing?”
- Schedule brief weekly check-ins for formal feedback discussions
- Receive criticism graciously without defensiveness or excuses
- Demonstrate implementation of previous feedback to show teachability
Steps to Communicate Effectively with Your Preceptor
- Weekly check-in structure:
- Review objectives achieved and those still in progress
- Discuss challenging cases or knowledge gaps encountered
- Request specific learning opportunities for upcoming week
- Address any concerns before they become significant problems
- Addressing concerns professionally: Use “I” statements to express difficulties without blaming, propose potential solutions rather than just identifying problems, remain open to preceptor perspectives, and document agreements in writing when appropriate
- Expressing gratitude effectively: Provide specific examples of valuable teaching moments, write thoughtful thank-you notes highlighting particular learning experiences, offer to present interesting cases you researched, and maintain professional connections beyond rotation end
Strategy #4 – How to Track Your Clinical Progress Systematically
Systematic tracking prevents last-minute scrambling to meet objectives and identifies gaps early enough to address them strategically.
- Digital versus paper tracking methods:
- Digital advantages: Cloud backup, easy sharing with faculty, automatic calculations, searchable databases
- Paper advantages: No technology barriers, immediate access without devices, personally tactile for kinesthetic learners
- Hybrid approach: Daily paper logs transferred weekly to digital spreadsheets
- Clinical log best practices:
- Record encounters immediately after completion while details remain fresh
- Include patient demographics, chief complaint, your differential diagnoses, treatment plan, and procedures performed
- Note objective(s) demonstrated during each encounter
- Track preceptor supervision level (observation, assistance, independence)
- Regular backup of all records to prevent catastrophic data loss
- Identifying objective gaps early: Review logs weekly against program requirements, identify missing patient populations or diagnoses, communicate gaps to preceptors to prioritize specific encounters, and create action plans for underrepresented categories
Strategy #5 – Ways to Learn from Every Patient Encounter
Deliberate reflection transforms routine encounters into powerful learning experiences that accelerate clinical reasoning development.
- Post-encounter reflection questions:
- What would I do differently if I saw this patient again?
- What surprised me about this case or challenged my assumptions?
- What evidence-based guidelines apply to this presentation?
- What questions arose that I need to research further?
- How does this patient’s presentation compare to textbook descriptions?
- Building clinical reasoning skills: Review your differential diagnoses for accuracy after final diagnosis confirmation, analyze which historical or physical findings proved most valuable, identify any cognitive biases that influenced your thinking, and discuss reasoning errors with preceptors as learning opportunities
Strategy #6 – How to Network and Learn from Peers
Your classmates represent invaluable resources for shared learning, emotional support, and collaborative problem-solving throughout challenging rotations.
- Study group strategies for objectives: Meet weekly to discuss difficult cases, quiz each other on clinical guidelines, share rotation tips and preceptor insights, and review each other’s documentation for improvement suggestions
- Sharing clinical experiences safely: Maintain strict HIPAA compliance by de-identifying all patient information, focus discussions on clinical learning rather than gossip, respect confidentiality regarding preceptor relationships, and create supportive rather than competitive group dynamics
Strategy #7 – Ways to Manage Stress and Avoid Burnout
Sustainable clinical excellence requires protecting your mental health and maintaining balance despite intense rotation demands.
- Self-care during intense rotations:
- Maintain consistent sleep schedules even during demanding weeks
- Preserve time for physical activity to manage stress and maintain health
- Continue social connections with non-nursing friends for perspective
- Practice mindfulness or meditation to manage clinical anxiety
- Seek counseling if rotation stress becomes overwhelming
- Work-life balance tips: Set firm boundaries around study time versus personal time, schedule regular breaks between rotation blocks, maintain hobbies and interests outside healthcare, recognize that perfection is impossible and good enough is often sufficient, and remember that struggling doesn’t indicate incompetence but rather normal learning progression
Fixing Common Problems: Why Clinical Objectives Aren’t Working and How to Troubleshoot
Even with excellent planning and effort, you’ll inevitably encounter obstacles that threaten your objective achievement. Recognizing and addressing these common problems quickly prevents small issues from derailing your entire rotation experience.
Problem #1 – Why You’re Not Seeing Enough Patients and How to Fix It
Limited patient exposure represents the most frustrating barrier to meeting clinical objectives, particularly in slower practice settings or with preceptors who don’t delegate appropriately.
- Common reasons for limited exposure:
- Preceptor hesitation to allow student involvement due to time pressures or liability concerns
- Slow practice volume in certain specialties or geographic locations
- Patients declining student participation during sensitive visits
- Scheduling conflicts or administrative barriers preventing full-day attendance
- How to advocate for more experience:
- Have honest conversations with preceptors about your specific objective requirements
- Offer to arrive early or stay late for additional patient opportunities
- Request to see overflow patients or those with longer appointment times
- Volunteer for procedures, phone triage, or other learning activities during downtimes
- Making the most of slower days:
- Conduct comprehensive chart reviews to understand patient populations
- Practice documentation by writing sample notes on observed cases
- Research clinical topics relevant to your rotation specialty
- Offer to complete administrative tasks to build preceptor goodwill
- Shadow other providers in the practice for diverse perspectives
Steps to Request More Clinical Opportunities
- Conversation starters with preceptors: “I’ve noticed I’m averaging 3 patients daily but need 5-6 to meet my program requirements. Could we discuss ways to increase my patient volume?”
- Alternative learning opportunities: Telehealth visits, nursing home rounds, hospital admissions, community health screenings, or shadowing experiences at affiliated facilities
- Documenting insufficient experience: Keep detailed attendance records and patient logs, communicate concerns to faculty early rather than at rotation end, and request program assistance finding supplemental opportunities if preceptor cannot provide adequate volume
Problem #2 – Why You Feel Overwhelmed by Objectives and Ways to Overcome It
Feeling overwhelmed occasionally is normal, but persistent anxiety that paralyzes learning requires immediate intervention.
- Distinguishing normal versus concerning anxiety:
- Normal: First-week jitters, pre-presentation nervousness, occasional self-doubt about clinical decisions
- Concerning: Panic attacks before clinical days, persistent insomnia, thoughts of quitting your program, complete confidence loss
- How to break objectives into micro-goals:
- Instead of “master physical examination,” focus on “perfect cardiac exam this week”
- Replace “develop clinical reasoning” with “formulate differential diagnoses for 3 chief complaints daily”
- Transform overwhelming semester objectives into daily achievable tasks
- When to seek faculty support: Contact your faculty immediately if anxiety persists beyond initial adjustment period, if preceptor relationships become toxic, if you’re falling significantly behind objective timelines, or if personal circumstances interfere with clinical performance
- Stress management techniques: Deep breathing exercises before patient encounters, positive self-talk replacing negative internal dialogue, recognizing that mistakes are learning opportunities not career-ending failures, and celebrating small victories rather than dwelling on perceived shortcomings
Worried Your Paper Won’t Meet Expectations?
StudentResearch.net guarantees satisfaction with unlimited free revisions. We refine your work until it perfectly aligns with your professor’s feedback and grading rubric. No risk, no compromise—just results that match your academic standards.
Problem #3 – Fixing Poor Preceptor-Student Relationships
Personality conflicts or communication breakdowns with preceptors create miserable rotation experiences and compromise learning quality.
- Communication strategies to try first:
- Schedule a private conversation to discuss expectations and concerns directly
- Use “I feel” statements rather than accusatory “you always” language
- Ask for specific feedback about behaviors you can modify
- Demonstrate receptiveness to criticism and willingness to change
- Clarify any misunderstandings about program requirements or objectives
- When to request preceptor change:
- If communication attempts fail repeatedly and relationship remains toxic
- If preceptor behavior becomes inappropriate or abusive
- If preceptor consistently provides inadequate supervision or teaching
- If safety concerns arise regarding patient care or your well-being
- Protecting your professional reputation:
- Remain professional regardless of preceptor behavior
- Document concerning incidents objectively without emotional language
- Never complain about preceptors to staff or patients
- Work through proper program channels for resolution
- Focus on learning despite difficult circumstances when possible
Problem #4 – What to Do When Behind on Clinical Hours and Objectives
Falling behind creates compounding stress, but strategic action plans can help you catch up without compromising quality.
- Creating a catch-up plan:
- Honestly assess how far behind you are and calculate required weekly progress
- Identify which objectives have shortest timelines and prioritize accordingly
- Request additional clinical days or extended hours if your schedule permits
- Focus intensively on gaps rather than spreading efforts across all objectives
- Working with program coordinators:
- Communicate deficits early when more solutions exist
- Provide documentation of attempts to meet requirements
- Be open to alternative rotation sites or schedule adjustments
- Understand that some programs require objective completion for progression
- Preventing future shortfalls: Track progress weekly rather than monthly, address concerns immediately rather than hoping they resolve, communicate proactively with preceptors about requirements, and build buffer time into your schedule for unexpected challenges
Essential Resources and Tools: What Nurse Practitioner Students Need to Track Clinical Objectives
Having the right resources and organizational systems dramatically improves your ability to track progress, identify gaps, and demonstrate competency achievement efficiently.
Best Tools and Templates for Tracking Clinical Objectives
Modern technology and well-designed templates streamline the administrative burden of clinical documentation, freeing mental energy for actual learning.
- Clinical objective tracking templates:
- Spreadsheet templates with formulas that calculate completion percentages automatically
- Paper logs with checkboxes for quick objective correlation during encounters
- Digital portfolios that organize evidence of competency by objective category
- Mobile apps designed specifically for NP student clinical tracking
- Recommended apps for NP students:
- Typhon or EXXAT: Clinical tracking platforms many programs require
- Medscape or Epocrates: Free drug references and clinical tools
- UpToDate: Gold-standard clinical decision support (check if your program provides access)
- Calculate by QxMD: Medical calculators for clinical decision rules
- Professional organization resources:
- AANP (American Association of Nurse Practitioners): Student membership provides networking, journals, and certification prep
- NONPF (National Organization of Nurse Practitioner Faculties): Competency standards and educational resources
- Specialty organizations (NAPNAP for pediatrics, NPWH for women’s health): Specialty-specific guidelines and practice resources
Free Resources Every NP Student Should Use
- Clinical guidelines databases:
- CDC.gov for immunizations, disease prevention, and public health guidelines
- USPSTF.org for evidence-based preventive care recommendations
- Guidelines.gov for comprehensive clinical practice guidelines across specialties
- Differential diagnosis tools: Isabel DDx, DiagnosisPro, or DXplain to expand diagnostic thinking
- Documentation templates: Many NP programs and textbooks include sample templates; adapt these to your learning style rather than creating from scratch
- Study guides for objectives: YouTube channels like FNP Mastery, podcasts like The Nurse Practitioner Show, and free webinars from professional organizations
How to Create Your Personal Clinical Success Plan
A personalized success plan transforms abstract objectives into concrete action steps with clear timelines and accountability measures.
- 30-day action plan template:
- Week 1: Establish preceptor relationship, understand clinic workflow, complete baseline objective assessment
- Week 2: Begin independent patient encounters with supervision, identify learning priorities
- Week 3: Increase patient volume and complexity, seek feedback on progress
- Week 4: Assess objective completion status, adjust strategies for remaining weeks
- Quarterly objective review schedule:
- Review transcript of objectives achieved versus program requirements
- Identify any categories underrepresented in clinical log
- Communicate gaps to upcoming rotation preceptors in advance
- Celebrate progress milestones to maintain motivation
- Post-graduation competency maintenance guide: Clinical learning doesn’t end at graduation; plan for ongoing professional development through journal subscriptions, conference attendance, specialty certifications, and collaborative practice arrangements that provide ongoing mentorship
Step-by-Step Action Plan Checklist
- Week 1 priorities:
- Meet with preceptor to discuss learning style, objectives, and expectations
- Understand clinic schedule, patient population, and documentation system
- Complete required paperwork, background checks, and immunization documentation
- Observe diverse patient encounters to understand workflow
- Monthly milestones:
- Month 1: Establish foundation skills and routine
- Month 2: Increase independence and patient complexity
- Month 3: Demonstrate consistent competency across objectives
- Final month: Function at near-independent practitioner level
- End-of-program goals:
- Complete all required clinical hours and patient encounters
- Demonstrate competency in all program-defined objectives
- Secure strong preceptor references for employment applications
- Feel confident in ability to practice independently
- Pass certification examination on first attempt
- Certification preparation integration: Align clinical objectives with certification exam content, seek diverse patient populations matching exam blueprints, practice clinical reasoning in exam format, and review high-yield topics throughout rotations rather than cramming afterward
Conclusion
You now have a comprehensive roadmap for mastering clinical objectives throughout your nurse practitioner education. From understanding the five core objective types to implementing proven achievement strategies and troubleshooting common problems, you possess the knowledge to transform clinical rotations from anxiety-inducing challenges into confidence-building opportunities. Remember that clinical competency develops progressively through consistent effort, not overnight perfection.
The most successful NP students share common characteristics: they engage actively with their objectives from day one, maintain systematic tracking systems, build strong preceptor relationships, and address problems quickly rather than hoping they resolve themselves. They recognize that struggling represents normal learning progression, not personal inadequacy. They seek help when needed and celebrate small victories along the journey toward independent practice.
Start implementing these strategies during your very next clinical day. Review your current objectives, create a tracking system that works for your style, prepare thoroughly before each rotation, and communicate openly with your preceptors about your learning needs. Download the free objective tracking template mentioned earlier, join a peer study group for accountability and support, and commit to weekly progress reviews that keep you on track.Learn clinical objectives for nurse practitioner students: 5 types, step-by-step goal setting, 7 strategies, and solutions to common rotation problems.
Your clinical objectives aren’t obstacles standing between you and graduation—they’re the scaffolding supporting your development into a competent, confident nurse practitioner. Each objective you achieve represents real patients you’ll serve more effectively, clinical situations you’ll navigate more safely, and professional challenges you’ll handle more competently throughout your career. Embrace the process, trust your growth, and remember why you chose this challenging yet incredibly rewarding profession.
You’ve got this. Now go show your next rotation what you’re capable of achieving.
Tired of Hidden Academic Service Fees? StudentResearch.net offers transparent pricing with zero surprises. Get an instant, final quote based on your deadline and academic level—guaranteed. Budget-conscious students deserve reliability. Know exactly what you’ll pay before committing to any service