Table of Contents
ToggleThe transition from a sterile classroom to the bustling, high-stakes environment of a hospital ward is the most exhilarating and terrifying moment in a nurse’s education. Clinical experience for nursing students is not just a requirement; it is the crucible where theoretical knowledge is forged into lifesaving intuition. Whether you are prepping for your first rotation or looking to sharpen your existing skills, mastering this phase is the key to becoming a confident healthcare professional.
Introduction to Clinical Excellence
The foundation of a successful career begins long before you graduate, rooted deeply in the hands-on practice found in hospital corridors. Clinical experience for nursing students serves as the vital bridge between textbook diagrams and the reality of patient care. In this guide, we explore how to navigate these rotations with precision, ensuring you emerge as a competent and compassionate caregiver.
Why Clinical Rotations Matter
- Real-world application: Transforming $vitals$ and $pathophysiology$ into actionable patient assessments.
- Professional socialization: Learning the unspoken language of the healthcare team and hospital culture.
- Confidence building: Reducing the “reality shock” often felt by new graduates entering the workforce.
Preparation and First Impressions
Walking onto a unit for the first time requires more than just a clean uniform; it requires a mindset geared toward proactive learning. Successful clinical experience for nursing students starts with rigorous mental and physical preparation to ensure you are ready for any scenario. By establishing a strong professional presence early, you earn the trust of your preceptors and patients alike.
The Pre-Shift Checklist
- Reviewing Patient Charts: Understanding the “why” behind every medication and procedure before the shift begins.
- Equipment Familiarity: Knowing where the crash cart, supply room, and vitals machines are located.
- Professional Attire: Ensuring your appearance reflects the high standards of the nursing profession.
Communication Skills
- SBAR Technique: Using Situation, Background, Assessment, and Recommendation for clear handoffs.
- Active Listening: Focusing entirely on the patient’s verbal and non-verbal cues.
- Conflict Resolution: Learning to navigate high-stress interactions with grace and professionalism.
Section 3: #1 Mastering Technical Nursing Skills
The ability to perform technical tasks with accuracy and empathy is a hallmark of a skilled nurse. During your nursing student clinical practice, you must seek out every opportunity to practice skills like IV starts, catheterizations, and wound care. Mastery comes through repetition, observation, and a willingness to step outside your comfort zone under supervision.
High-Frequency Clinical Skills
- Medication Administration:
- H4: The Five Rights:
- Right Patient: Always use two identifiers.
- Right Drug: Triple-check the MAR.
- Right Dose: Recalculate if something feels off.
- Right Route: Ensure the delivery method is appropriate.
- Right Time: Adhering to the specific window for efficacy.
- H4: The Five Rights:
- Wound Management: Identifying stages of pressure ulcers and applying sterile dressings.
- Phlebotomy and IVs: Mastering the art of vein selection and aseptic technique.
Utilizing Student Research in Practice
- Evidence-Based Practice: Incorporating student research to understand the latest protocols in infection control.
- Protocol Comparison: Evaluating hospital policy against current academic literature.
- Continuous Learning: Asking your preceptor for the “latest evidence” behind specific unit-based interventions.
Struggling with complex dosage math or care plans? Don’t let academic stress hinder your clinical growth. Get expert help with your nursing papers at StudentResearch.net. We provide precise, high-quality writing support to ensure your academic success matches your clinical skills!
#2 Critical Thinking and Clinical Judgment
Developing clinical judgment is perhaps the most difficult yet rewarding aspect of your education. Clinical experience for nursing students challenges you to look past the obvious symptoms to find the underlying cause of a patient’s distress. By asking “what if” and “why now,” you develop the foresight necessary to prevent adverse events before they occur.
The Nursing Process in Action
- Assessment: Gathering comprehensive data through head-to-toe examinations.
- Diagnosis: Identifying human responses to health conditions.
- Planning: Setting SMART (Specific, Measurable, Achievable, Relevant, Time-bound) goals for patient recovery.
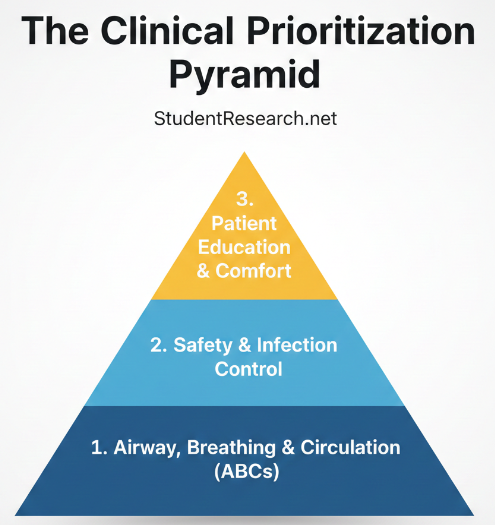
Prioritization Strategies
- ABC (Airway, Breathing, Circulation): Always addressing life-threatening issues first.
- Maslow’s Hierarchy: Ensuring basic physiological needs are met before addressing psychological ones.
- Time Management: Mapping out your shift to balance patient care, documentation, and breaks.
Clinical Nurse Rotation Example
Transitioning into a Pediatric clinical rotation requires a shift in both your clinical mindset and your communication style. Unlike adult patients, pediatric care involves “family-centered care,” where you are treating the child while simultaneously managing the expectations and anxieties of the parents.
The following schedule is designed to help you balance the technical requirements of the unit with the developmental knowledge needed to excel in this specialty.
4-Week Pediatric Clinical Mastery Schedule
Week 1: Developmental Milestones and Safety
The first week is about understanding “normal” for different age groups. A 2-year-old’s vitals and behavior are vastly different from a 12-year-old’s.
- Study Focus: Review Erikson’s Stages of Psychosocial Development and Piaget’s Cognitive Theory.
- Clinical Goal: Practice the “least invasive to most invasive” assessment technique (e.g., listen to heart/lung sounds while the child is quiet before checking their ears or throat).
- Key Skill: Calculating safe pediatric dosages (mg/kg) for common medications like Acetaminophen or Ibuprofen.
- Student Research Task: Look up the hospital’s specific “Safe Sleep” policies for infants and how they align with current American Academy of Pediatrics (AAP) guidelines.
Week 2: Respiratory and Fluid Management
Respiratory issues are the primary reason for pediatric admissions. This week, focus on the unique anatomy of a child’s airway and their high risk for dehydration.
- Study Focus: Common pediatric conditions: RSV, Asthma, Croup, and Epiglottitis.
- Clinical Goal: Identify signs of respiratory distress (nasal flaring, grunting, retractions).
- Technical Skill: Monitor IV fluid rates and “Burette” safety; children have a much lower threshold for fluid overload.
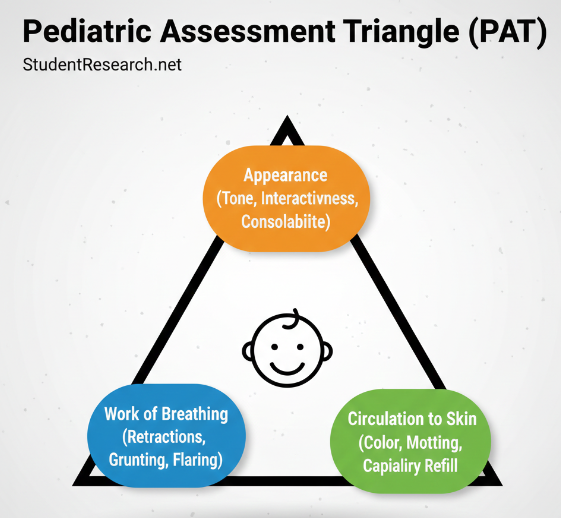
- Visual Aid:
Week 3: Family-Centered Care and Chronic Conditions
In week three, you should focus on the “Family” part of the equation. You will likely encounter children with chronic illnesses like Type 1 Diabetes or Cystic Fibrosis.
- Study Focus: Chronic disease management and the impact of hospitalization on the family unit.
- Clinical Goal: Lead a teaching session with a parent (e.g., how to use an inhaler or administer home medications).
- Student Research Task: Investigate the role of “Child Life Specialists” and how their interventions improve clinical outcomes for hospitalized children.
- Communication Skill: Practice “Medical Play”—using dolls or equipment to explain procedures to a child in a non-threatening way.
Week 4: Critical Thinking and Emergency Response
Your final week is about “putting it all together” and recognizing the “flicker”—the subtle signs that a child is deteriorating.
- Study Focus: Pediatric Advanced Life Support (PALS) basics and the Pediatric Assessment Triangle (Appearance, Work of Breathing, Circulation).
- Clinical Goal: Take on a “full patient load” (as allowed by your instructor) to practice time management between multiple pediatric patients.
- Student Research Task: Review a case study on “Pediatric Sepsis” to identify the early warning signs specific to the pediatric population.
Pediatric Comparison: Vital Signs by Age
Use this table as a quick reference during your shift to ensure you are interpreting vitals correctly.
| Age Group | Heart Rate (BPM) | Respiration Rate | Systolic BP (mmHg) |
| Newborn | 100–180 | 30–60 | 60–90 |
| Toddler (1-3y) | 80–110 | 24–40 | 90–105 |
| School Age (6-12y) | 70–110 | 18–30 | 100–120 |
| Adolescent (13y+) | 60–90 | 12–16 | 110–130 |
Tip for Success
Always remember: Parents are the experts on their child. If a parent tells you their child “just doesn’t look right” or is “acting different,” take it seriously. It is often the first sign of a clinical change that won’t show up on a monitor for another hour.
Mastering pediatric dosage calculations is all about precision, as even a small decimal error can have significant consequences. In pediatrics, almost every dose is weight-based, typically calculated in mg/kg.
Here are 10 practice problems ranging from basic weight conversions to complex IV flow rates.
Pediatric Dosage Practice Problems
- Weight Conversion: A toddler weighs 28 lbs 4 oz. Convert this weight into kilograms. (Round to the nearest hundredth).
- Basic Oral Liquid: An order reads: Amoxicillin 125 mg PO every 8 hours. The pharmacy provides a bottle labeled 250 mg/5 mL. How many mL will you administer per dose?
- Weight-Based Dose: A child weighs 15 kg. The physician orders Cefazolin 25 mg/kg IV. How many mg will you administer for one dose?
- Safe Dose Range (SDR): A child weighs 22 kg. The SDR for a specific antibiotic is 20–40 mg/kg/day divided into two doses. What is the minimum and maximum single dose (in mg) this child can safely receive?
- Liquid Suspension: A physician orders Motrin 10 mg/kg for a child weighing 31 lbs. The concentration available is 100 mg/5 mL. How many mL should the parent give?
- IV Bolus: An order is for a Normal Saline bolus of 20 mL/kg over 30 minutes for a dehydrated infant weighing 6.2 kg. What is the total volume to be infused?
- IV Flow Rate: You need to infuse 250 mL of D5W over 4 hours. Using a microdrip set (60 gtt/mL), what is the flow rate in drops per minute (gtt/min)?
- Multi-Step Calculation: A doctor orders Gentamicin 3 mg/kg/day IV to be given in three divided doses. The patient weighs 44 lbs. The medication is supplied as 20 mg/2 mL. How many mL will you give per dose?
- Safe Dose Evaluation: A child weighing 18 kg is prescribed 450 mg of a drug every 12 hours. The SDR is 40–60 mg/kg/day. Is this dose safe? (Show your math).
- Maintenance Fluids: Using the 100/50/20 rule, calculate the 24-hour maintenance fluid requirement for a child weighing 24 kg.
Answer Key & Formulas
| Problem | Answer | Calculation Pathway (for your review) |
| 1 | 12.84 kg | $4 oz / 16 = 0.25 lbs \rightarrow 28.25 / 2.2 = 12.84 kg$ |
| 2 | 2.5 mL | $(125 / 250) \times 5 mL$ |
| 3 | 375 mg | $15 kg \times 25 mg$ |
| 4 | 220–440 mg | $Min: (22 \times 20)/2 = 220; Max: (22 \times 40)/2 = 440$ |
| 5 | 7.05 mL | $31 lbs / 2.2 = 14.09 kg \rightarrow (140.9 / 100) \times 5$ |
| 6 | 124 mL | $20 mL \times 6.2 kg$ |
| 7 | 62 gtt/min | $(250 mL \times 60) / 240 mins$ |
| 8 | 2 mL | $20 kg \times 3 mg = 60 mg/day \div 3 doses = 20 mg/dose$ |
| 9 | Yes (Safe) | $SDR: 720–1080 mg/day. Ordered: 900 mg/day.$ |
| 10 | 1,580 mL | $(10 \times 100) + (10 \times 50) + (4 \times 20) = 1580$ |
Study Tip: The 100/50/20 Rule
For Problem #10, remember the standard pediatric maintenance fluid formula:
- First 10 kg: $100 mL/kg$
- Next 10 kg: $50 mL/kg$
- Each kg over 20: $20 mL/kg$
The 100/50/20 Rule (also known as the Holliday-Segar Method) is the gold standard for calculating a pediatric patient’s 24-hour maintenance fluid requirement. Because children have a higher metabolic rate and larger body surface area relative to their weight than adults, their fluid needs must be calculated with extreme precision to prevent dehydration or fluid overload.
Breaking Down the Holiday-Segar Method Rule
This rule breaks a child’s total weight into three “brackets.” You calculate the fluid for each bracket and then add them together for the Total Daily Volume.
- First 10 kg of body weight: Give 100 mL/kg.
- Next 10 kg of body weight (11–20 kg): Give 50 mL/kg.
- Each kg over 20 kg: Give 20 mL/kg.
Step-by-Step Examples
Example 1: The 8 kg Infant (Bracket 1 only)
Since this child is under 10 kg, we only use the first part of the rule.
- $8 kg \times 100 mL = 800 mL/24 hours$
- Hourly Rate: $800 / 24 = 33.3 mL/hr$
Example 2: The 15 kg Toddler (Brackets 1 and 2)
We must “fill” the first bracket before moving to the second.
- First 10 kg: $10 \times 100 = 1,000 mL$
- Remaining 5 kg: $5 \times 50 = 250 mL$
- Total Daily Volume: $1,000 + 250 = 1,250 mL/24 hours$
- Hourly Rate: $1,250 / 24 = 52 mL/hr$
Example 3: The 32 kg School-Age Child (All 3 Brackets)
This uses the full weight distribution.
- First 10 kg: $10 \times 100 = 1,000 mL$
- Second 10 kg: $10 \times 50 = 500 mL$
- Remaining 12 kg: $12 \times 20 = 240 mL$
- Total Daily Volume: $1,000 + 500 + 240 = 1,740 mL/24 hours$
- Hourly Rate: $1,740 / 24 = 72.5 mL/hr$
The “4-2-1” Shortcut
During a busy clinical experience for nursing students, you might not have time to calculate the full 24-hour volume first. Many nurses use the 4-2-1 Rule to find the hourly rate directly:
- 4 mL/hr for the first 10 kg.
- 2 mL/hr for the next 10 kg.
- 1 mL/hr for every kg over 20.
Example (32 kg child):
$(10 \times 4) + (10 \times 2) + (12 \times 1) = 40 + 20 + 12 = 72 mL/hr.$
(Note: The slight difference from 72.5 is due to rounding in the 24-hour method, but 4-2-1 is the standard for setting IV pumps quickly.)
Why This Matters in Your Rotation
As part of your student research into patient safety, you’ll find that pediatric patients are highly sensitive to “Insensible Water Loss” (fever, tachypnea, sweating). If a child has a high fever, the provider might order “1.5x Maintenance” fluids. You would simply calculate the base maintenance and multiply the final result by 1.5.
Top 5 Mistakes to Avoid During Clinical Rotations
Making mistakes is a natural part of the learning process, but in the healthcare environment, some errors carry more weight than others. During your clinical experience for nursing students, being aware of common pitfalls allows you to proactively guard against them, ensuring both patient safety and your professional reputation.
Here is a checklist of the top 5 mistakes to avoid to ensure you remain a high-performing student on any unit.
The Top 5 Mistakes to Avoid Checklist
- #1: Faking It Until You Make It
- The Risk: In nursing, “guessing” can be fatal. If you are unsure about a medication, a procedure, or a patient’s change in status, never stay silent.
- The Fix: Always ask for clarification. Preceptors respect a student who knows their limits more than one who takes dangerous risks.
- #2: Neglecting the “Basics” (ADLs)
- The Risk: Many students focus so much on “cool” skills like IV starts that they ignore Activities of Daily Living (ADLs) like bathing, feeding, and turning patients.
- The Fix: Use ADLs as your primary assessment time. You can learn more about a patient’s skin integrity, respiratory effort, and cognitive status while giving a bed bath than you can by just reading a chart.
- #3: Poor Time Management and “Tunnel Vision”
- The Risk: Getting stuck in one room for an hour while your other patients’ needs go unmet.
- The Fix: Use a “Brain Sheet” to track your entire assignment. Check in on every patient at the start of the shift so you can prioritize based on acuity rather than whoever called the light first.
- #4: Violating Professional Boundaries (Social Media & HIPAA)
- The Risk: Posting “vague” stories about your shift or taking photos in the hospital, even if no patient names are visible.
- The Fix: Keep your phone in your locker. HIPAA violations are often grounds for immediate dismissal from a nursing program and can prevent future licensure.
- #5: Disregarding the Multidisciplinary Team
- The Risk: Viewing the nursing role in a vacuum and ignoring the input of CNAs, Respiratory Therapists, or Physical Therapists.
- The Fix: Treat the nursing assistants with the utmost respect—they often know the patients better than anyone else on the floor. Listen to the RTs when they explain ventilator settings; this is where the best student research happens in real-time.
#3 Emotional Intelligence and Patient Advocacy
Nursing is as much an art of the heart as it is a science of the mind. During your clinical experience for nursing students, you will encounter patients at their most vulnerable, requiring you to be their voice. Balancing clinical detachment with genuine empathy is a skill that will define your career longevity and patient satisfaction.
Cultivating Empathy
- Therapeutic Communication: Using open-ended questions to encourage patients to share their concerns.
- Cultural Competency: Respecting diverse backgrounds and tailoring care to meet specific cultural needs.
- Patient Advocacy: Speaking up when a patient’s wishes are not being fully addressed by the medical team.
Managing Stress and Burnout
- Self-Care Rituals: Developing habits that help you decompress after a difficult shift.
- Peer Support: Utilizing your cohort to discuss challenging clinical cases and emotional hurdles.
- Reflective Journaling: Writing down your experiences to process emotions and track professional growth.
#4 Comparative Analysis of Clinical Settings
Not all clinical rotations are created equal, and understanding the nuances of each can help you find your niche. This section provides a comparative look at the different environments you might encounter during your clinical experience for nursing students. From the fast-paced ICU to the community-focused clinic, each setting offers unique learning opportunities.
Comparing Clinical Environments
| Feature | Med-Surg Units | Critical Care (ICU) | Community/Public Health |
| Patient Ratio | 1:5 – 1:7 | 1:1 – 1:2 | Varies (Population focused) |
| Skill Focus | Time management & Multi-tasking | Advanced Tech & Hemodynamics | Education & Prevention |
| Pace | High-volume, steady | Intense, unpredictable | Moderate, scheduled |
| Research Role | Routine student research application | High-level student research on acuity | Epidemiological student research |
Maximizing Each Rotation
- Specialty-Specific Goals: Setting unique objectives for every new unit you visit.
- Networking: Building relationships with nurses in specialties you find interesting.
- Cross-Training: Observing how different departments (Radiology, Lab, Pharmacy) interact with nursing.
Is evidence-based practice weighing you down? Transforming clinical observations into A+ research papers is our specialty. Visit StudentResearch.net today for professional assistance with your nursing essays. We handle the deep research so you can focus on mastering your bedside care!
#5 Documentation and Professionalism
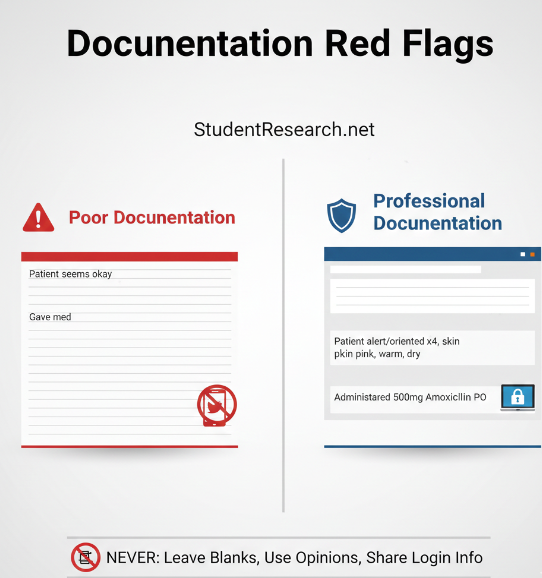
If it wasn’t documented, it wasn’t done—this is the golden rule of nursing that you must master early. Your clinical experience for nursing students will involve learning various Electronic Health Record (EHR) systems and the legalities of medical charting. Professionalism extends beyond the chart, encompassing how you interact with the entire multidisciplinary team.
Documentation Best Practices
- Objectivity: Recording what you see, hear, and do, rather than your personal opinions.
- Timeliness: Charting as close to the event as possible to ensure accuracy.
- Legal Safeguards: Understanding the implications of HIPAA and patient privacy in a digital world.
Interdisciplinary Collaboration
- Team Meetings: Participating in multidisciplinary rounds to gain a holistic view of patient care.
- Role Clarity: Understanding the specific functions of PT, OT, RT, and Social Work.
- Professional Boundaries: Maintaining a therapeutic relationship with patients and their families.
#6 Conclusion
As you wrap up your rotations, take a moment to reflect on the immense growth you have achieved. Clinical experience for nursing students is a journey of continuous improvement, and every mistake is a lesson, while every success is a building block. Carry these examples of excellence into your future career, and never stop seeking the mastery of your craft.
Final Summary of Tips
- Stay Curious: Never stop asking “why” during your clinical hours.
- Be Proactive: Volunteer for the tasks that others shy away from.
- Review and Reflect: Use your clinical evaluations to target areas for improvement.
Meta Description: Master your clinical experience for nursing students with these 6 expert tips. Gain skills, see examples, and achieve mastery in patient care today